Part of the Valentines week
Prep work:
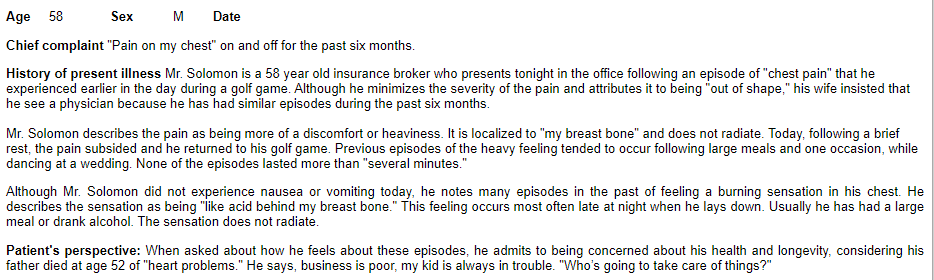
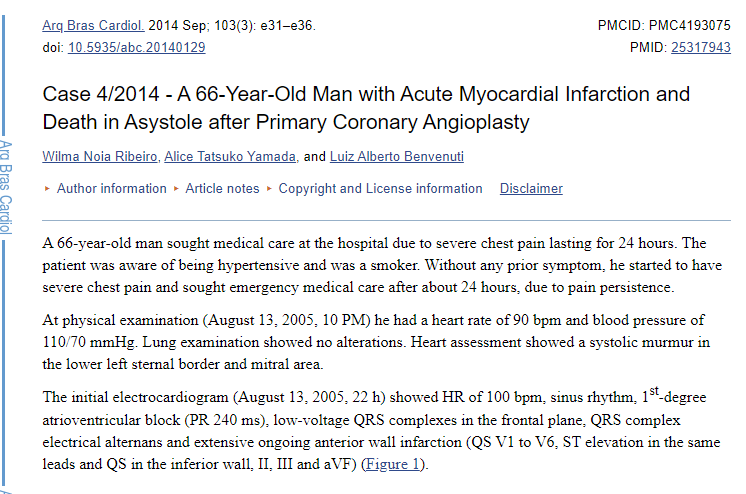
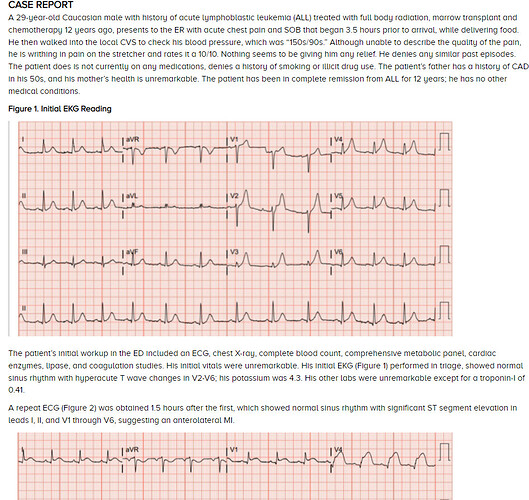
- Start with clinical description here - key insights
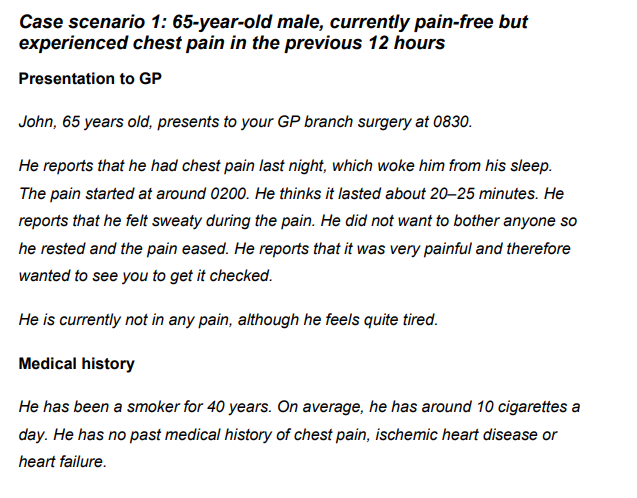
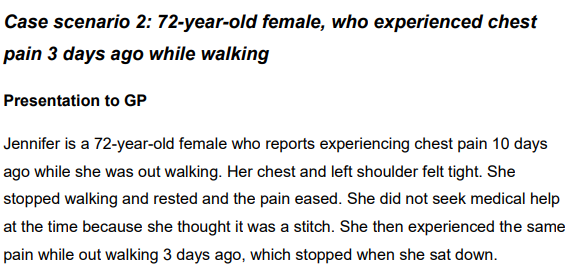
- Review clinical vignettes to understand the phenotype from an individual patient or treating clinician perspective.
Key insight:
- There are significant difference in experiences based on whether it is UA/NSTEMI/STEMI from patients perspective.
- People may be hospitalized with suspected cases of Myocardial Infarction.
- Literature review - understand prior work
Key insights:
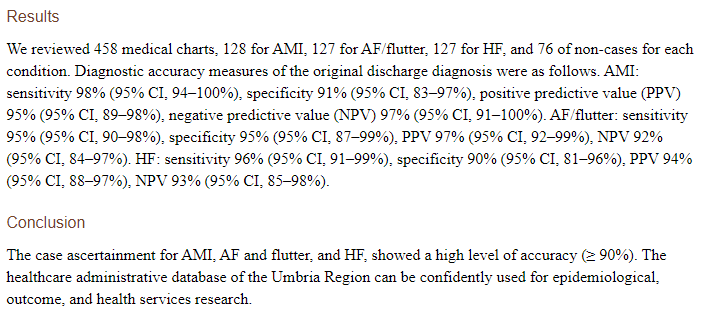
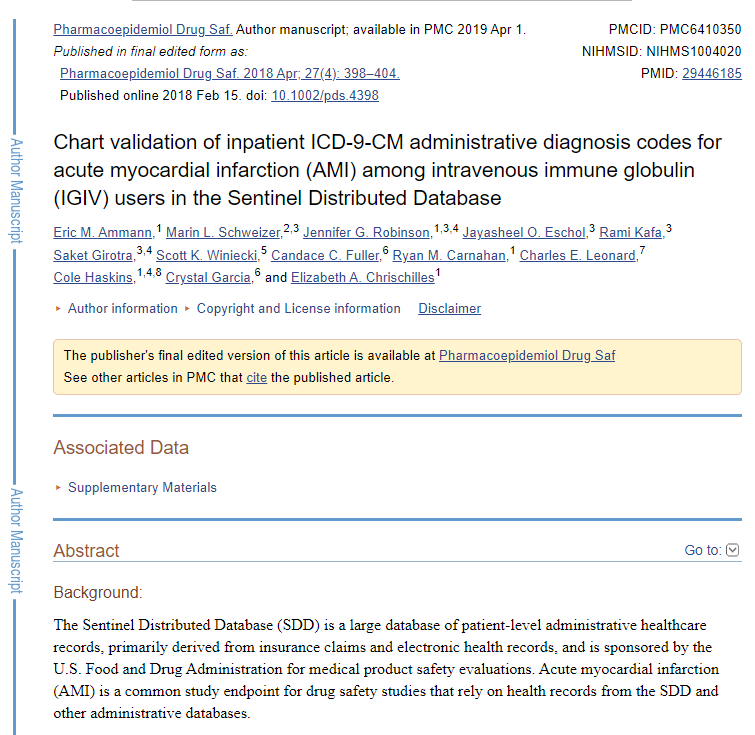
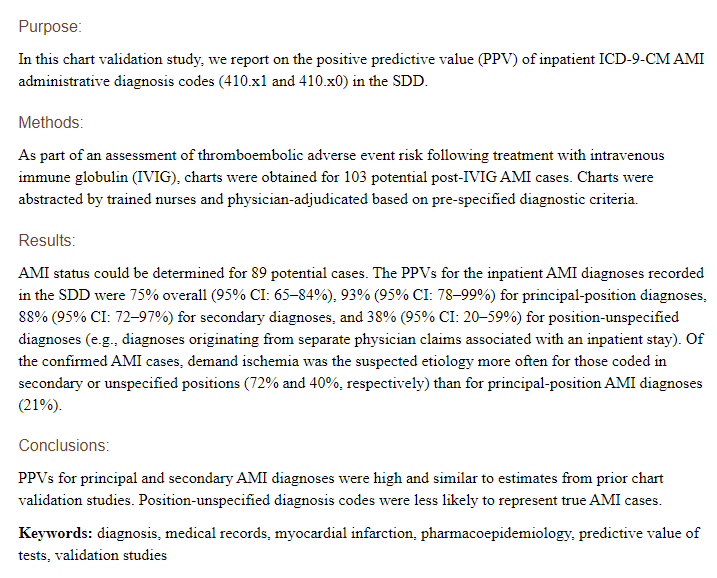
- Most publications document good validity of cohort definitions. There has been significant prior work
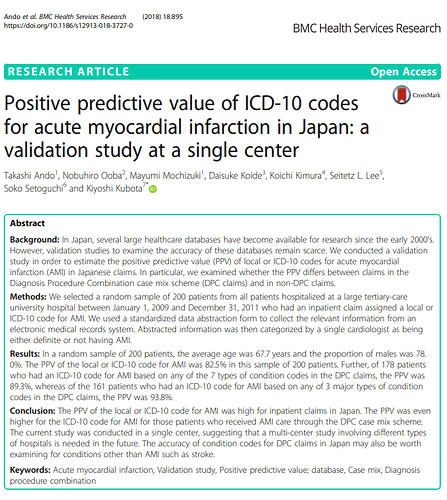
- We reviewed the codes used in the definitions from prior studies. Most have removed Old MI related codes from the entry event criteria - there is debate about the use of “subsequent” MI codes here and here and is currently unresolved. How would we generate empirical data to support this decision? Should we keep or not keep subsequent MI codes.
Phenotypes:
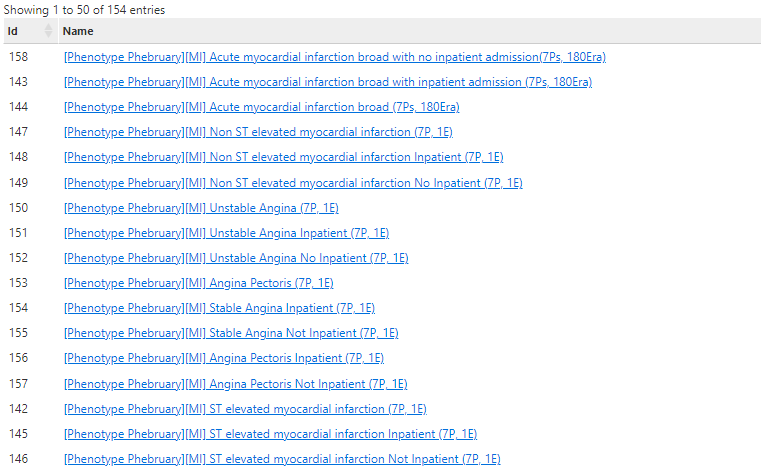
- A starting set of cohorts (3 each) for Angina pectoris, unstable angina, NSTEMI, STEMI and Acute MI were built - and are in https://data.ohdsi.org/phenotypePhebruary/ and ATLAS . Evaluation is being done using the framework described here
The paper attempts to structure the evaluation to detect three types of errors - and the evaluation below will follow that framework.
Sensitivity error - we may say that a given cohort has sensitivity errors, if we observe evidence that there are persons in the data source who may have the phenotype of interest but are not identified by the PA.
Specificity error - we may say that a given cohort has specificity errors, if we observe evidence that subjects identified by the PA do not have the phenotype of interest.
Index-date misclassification - we may say that a given cohort has index-date misclassification error, if we observe evidence that subjects identified by the PA have incorrect designation of event start date.
- Evaluation of phenotypes using Cohort Diagnostics at https://data.ohdsi.org/phenotypePhebruary/
- Evaluation of phenotypes for Acute Myocardial Infarction
- Evaluation of phenotypes for ST Elevation Myocardial Infarction
- Evaluation of phenotypes for Non ST elevation Myocardial Infarction
- Evaluation of phenotypes for Unstable Angina
- Evaluation of phenotypes for Chronic Stable Angina
- Evaluation of relationships between Acute MI/STEMI/NSTEMI/UA/Chronic Angina phenotypes
Key points:
- I like to start with cohort definitions that capture the occurrence of the cohort for the first time in persons history, evaluate those cohorts and then decide if the definitions can be changed to allow multiple records per person.
- Since this phenotype is an acute event that is expected to be managed (per clinical description) in a hospital - datasources that do not have inpatient records will not be considered in this evaluation (because these datasource maybe expected to have sensitivity errors by not capturing persons experience while in hospital)