1. C. Look at clinical vignettes - to understand the perspective of a treating clinician
Source: https://www.nice.org.uk/guidance/qs28/resources/clinical-case-scenarios-pdf-247324717
Clinical case scenarios: Hypertension (2013)
| OHDSI Home | Forums | Wiki | Github |

1. C. Look at clinical vignettes - to understand the perspective of a treating clinician
Source: https://www.nice.org.uk/guidance/qs28/resources/clinical-case-scenarios-pdf-247324717
Clinical case scenarios: Hypertension (2013)
1. D. Write a clinical description
This is definitely the most important step - and the place i generally spend the most amount of time. This is the “target” we are trying to phenotype - and if we don’t all have a shared understanding of what we are trying to phenotype - we can not “evaluate” if we are truly identifying the people we want to study in our cohort definitions.
I describe this to be a clinician’s description of a group of persons (patients) current externally observable clinical state. It is expected to be a verbose semi-structured description specified in natural human language, and this is not a computer algorithm or diagnosis code. In fact, at this stage - the phenotyper should NOT be even thinking of implementing the description as either a concept set or cohort definition. If a phenotyper is thinking of codesets NOW - stop - reset - restart. You dont know what you are phenotyping - so dont think of codesets!
My way of introducing structure to this step is by following the same structure that has been used for years in medical training - requiring the following components - Overview, Presentation, Assessment, Plan and Prognosis. Each component is expected to contain at-least one or two lines of clinical knowledge that was synthesized by clinicians (preferably by a panel) with medical knowledge, harvested from authoritative sources like medical text books.
Here are some examples I wrote for phenotyping purposes:
Vitiligo:
Overview: Vitiligo is the most frequent cause of acquired depigmentation disorder of skin that is characterized by development of well-defined white macules on the skin.
Presentation: Vitiligo typically presents with asymptomatic patches of skin that is milky/chalky white in color without signs of inflammation. Although it can appear at any age or anywhere on the body, it has predilection for the face, around orifices, in genitals, and hands. Depigmentation of hair may also occur. Most commonly Vitiligo is non-segmental but can be segmental too especially around the trigeminal nerve distribution.
Assessment: Clinical diagnosis is straightforward based on history and clinical examination. Routine skin biopsy is not needed.
Plan: If rapid progression is suspected, low-dose oral corticosteroids. Phototherapy may cause stabilization.
Prognosis: Clinical course is variable, may remain stable or slowly progress – with extent and distribution changing over lifetime.
Chronic lymphoid leukemia:
Overview: Mature B cell neoplasm characterized by a progressive accumulation of monoclonal B lymphocytes. Similar to non-Hodgkins lymphoma SLL, but the key difference is that this disease manifests primarily in blood, while SLL in primarily lymph node.
Presentation: Most commonly asymptomatic and detected on routine blood test with abnormal lymphocytosis. Occasionally there may be constitutional symptoms like unexplained weight loss, fevers, night sweats, fatigue. CLL does not have lymphadenopathy while non-HL/SLL does.
Assessment: Suspected when there is absolute lymphocytosis on peripheral smear. peripheral blood/bone marrow cell counts, immunophenotypic analysis (flow cytometry), bone marrow biopsy/aspirate, lymph node biopsy/aspirate, spleen.
Plan: Depends on activity of disease/stage; the disease is extremely heterogenous. Nodal disease may involve radiation therapy. There is no single agreed first line therapy.
Prognosis: Chronic disease but may be asymptomatic with minimal progression, or may progress quickly
Lichen planus
Overview: is a rare disease affecting middle aged adults most commonly affecting skin as pruritic, purple, polygonal and papular lesions lasting a few millimeters each, that may coalesce to forms large lesions over time. Common areas of extremities, scalp and genitalia. It may also involve the mucus members of the oral cavity and esophagus. It is commonly associated with hepatitis C.
Presentation: development of pruritic, purple, polygonal, papular lesions in the extremities that are few millimeters in size.
Assessment: clinical examination, no specific testing
Plan: no recommended treatment. Options include corticosteroids, phototherapy.
Prognosis: commonly remits over few years
We cannot phenotype decision:
For me the main indication is - if clinicians are unable to clearly write the clinical idea in this structure - then more than likely this is something we cannot phenotype. Also - if a (panel of) clinician are unable to agree on the clinical description - then we cannot phenotype.
1. D 2 - formalize the structure of clinical description
What should be in the clinical description
Minimum content:
Overview: is a key summary of the phenotype that highlights its salient features.
Presentation: is how the person or their clinician would first observe their phenotype.
Assessment: Once a person presents what would the clinician like to do to affirm diagnosis.
Plan: Assessment is likely to be followed by management plan - that is based on the patient preferences and established evidence.
Prognosis: Describes the expected future state, or the natural history of the phenotype – specifically how long will it last, what is expected to make it better or go away, what is expected to make it worse or become something else?
Additional content (recommended content - that i am still struggling with on how to formalize):
Similar outcomes: Are there phenotypes that are considered similar to the main phenotype of interest - that may co-exist or exclude the main phenotype? In medical practice, this is similar in idea to ‘differential diagnoses’. Conditions that may closely resemble the primary outcome but may not be the primary outcome of interest (overlapping conditions are acceptable, it does not have to be mutually exclusive). Note: this list does not have to be comprehensive, but we only need the top 2 or 3 key common differential diagnosis.
Examples
Chronic Lymphoid Leukemia:
- Non hodgkins leukemia
- Mantle cell lymphoma
Vitiligo:
- Tinea versicolor
- Scleroderma
Patient factors that are NOT expected to occur with the phenotype of interest:
Patient factors that are expected to occur with the outcome of interest:
What else do we know about the outcome of interest: This is a catch all section, try to capture any other relevant known information.
Acceptance criteria:
I have struggled here - and would love the community input on this topic. Can we define an “acceptance criteria” here - upfront, even before we start building concept sets?
For this phenotype - after much deliberation - the panel of clinicians decided to call this “Essential hypertension”" and clarified that it is not secondary hypertension, not malignant hypertension or hypertensive emergency and it is not Treated hypertension.
Essential Hypertension:
Overview: Persons newly (first time) diagnosed with chronic hypertension not explained by secondary/medically correctable causes, identified in an ambulatory/office setting as part of routine (asymptomatic)/incidental primary care visit in persons who have had no significant past medical history. No evidence of end organ damage.
Assessment: Ambulatory/home blood pressure measurements. Screen for secondary causes.
Plan: Treatment is almost always expected to be started AFTER initial diagnosis. Routine follow-up - more frequently initial as treatment is titrated. Less frequent if stable, responsive to treatment and well tolerated.
Prognosis: Variable - chronic disease, no end date.Similar outcomes:
Should not co-exist: Hyperaldosteronism, coarctation of the aorta, renal artery stenosis, chronic kidney disease, and aortic valve diseaseShould not occur with the phenotype:
Patient should not be worked up as an emergency (including inpatient hospital) - this is not a life threatening emergency.
Should not have been previously treated with blood pressure medication - treatment should ideally start AFTER diagnosis
No treatment in past - because not treated hypertension.
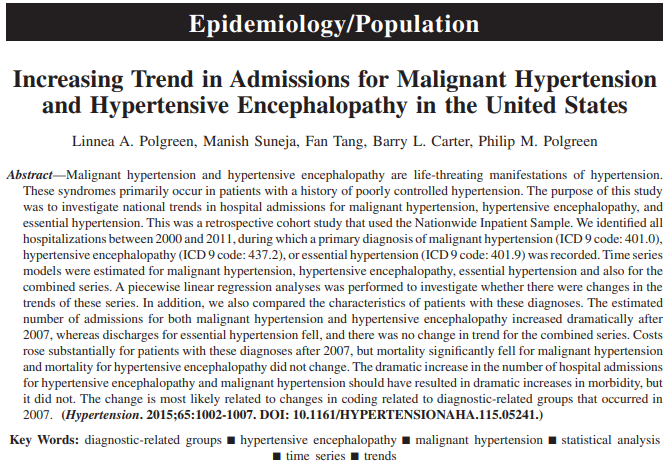
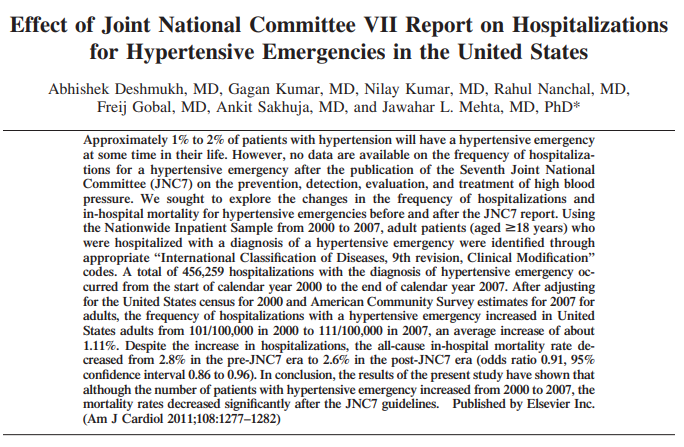
Not Malignant hypertension, resistant hypertension, hypertensive encephalopathy
Please read this clinical description together with the clinical notes above
Step 2: Perform a literature review.
The purpose of this section is to understand how others have tackled the problem of phenotyping in their work for observational research. This would be the first time - we start thinking of how to phenotype (ie. build concept set, build cohort definitions).
If you thought of or worked on concept sets/code sets/cohort definitions - prior to this step. STOP - RESET - REDO. 
Ideally - the panel who worked on the clinical description should also have provided the literature - but sometimes that is not the case. Also - this obviously may not be comprehensive - so if others know of a high quality work that needs to be part of this review - please post.
- Literature review: have others performed epidemiological/observational research-based studies on the outcome of interest. Are there published literature available that have studied the outcome of interest in observational data? Have they described how they developed an operational definition for the outcome of interest?
Capturing some key literature and insights below:
aged 18 years or older who were discharged from an ED with a primary discharge diagnosis of hypertension as defined by ICD-9-CM (International Classification of Diseases, 9th Revision, Clinical
Modification) codes 401-405.
Step 2: Perform a literature review.
I found the literature search pretty interesting - and raised a question/concern:
Some key insights:
My next step was to review the code set here - and review found
I found the review of AHRQ CCS codes interesting because “Hypertension and hypertensive-related conditions complicating pregnancy; childbirth; and the puerperium” was considered part of “Essential Hypertension”.
What does the community think? My position would be:
If you are reading till here - you probably are beginning to relate to a journey
By developing the clinical description - we now have a clearer understanding of what we are phenotyping. We have described a structure on how to develop such a clinical description
a) start with an authoritative sources that is at the right level - make your notes
b) review clinical vignettes - to better understand what it is, what it is not.
c) write clinical description - preferably a panel of clinicians - get consensus. If no consensus - then you cannot phenotype. If consensus - understand what it is, what if present would make it less likely/exclude it
d) develop an acceptance criteria
e) look and learn from others work in observational research - clarify any surprises (e.g. the pregnancy, primary vs secondary)
If you have looked at Altas or talked about codes PRIOR to reaching here - you are NOT following best practice  STOP - RESET - RESTART
STOP - RESET - RESTART
Now to build a concept set expression - we have a process for that appears to work. I wrote a paper on the Science Of Phenotyping here - that i don’t know if we can/cannot publish. Its part of the OHDSI Phenotype Development and Evaluation workgroup - if you want to contribute/collaborate on that work, please ping me (it describes/defines the phenotype development process). Most of the introduction content in that paper - i consider obsolete (represents our thinking in 2020)- because our thinking has evolved - but there are other sections that are still current.
Some excerpts from that paper
Step 3: Building Concept Set expression
The process to build concept set expression is described above (its not perfect, and there is an opportunity to document it better) - and was demonstrated by others during the Phenotype Phebruary @Patrick_Ryan and @AzzaShoaibi
But the key ideas are:
Few gotchya
Got an example?
Thanks @Gowtham_Rao for initiating the discussion on hypertension. Glad that we are talking about heart diseases on Valentines day 
One thing I am unclear about in this clinical description (and indeed most others), which I presume would fit under ‘prognosis’, is how to think about potential resolution of a condition, and whether this is expected or observable. In this example, we could consider hypertension as a chronic disease and assume its therefore a condition that continues indefinitely (so cohort end is end of observation period). But, that may be overly simplistic: generally, clinicians will advise lifestyle changes (diet and exercise) and some patients who control blood pressure in this manner may get to a point where they can stop treatment (or potentially never start). Same would go for t2dm, even though we generally think of that as a chronic disease with no end date. The first question in my mind, before looking in the data, is what is the clinical truth of the disease: is it truly chronic and unresolvable, or can it start and stop/ recur? Then, the follow up based on the data is: how do we model this clinical reality, given what is observable? I could imagine that we reach a conclusion that we cant find the proper cohort episodes with what data we have, but i dont want to confuse that with what should be a patients true time varying disease status.
Step 3 Building concept set expression
using lexical search, concept recommender, my re-reading of clinical description - i ended up with this concept set expression
Briefly - the way i got here
I did a lexical search for ‘hypertension’ and picked up
Upon looking at the resolved concept set - i found the concepts who also had parents to Hypertensive crisis, so i decided to exclude the parent.
Labile essential hypertension is mapped to Intermittent hypertension and is usually a type of Secondary hypertension - so based on clinical description - these are not part of the phenotype of interest.
Now to PHOEBE - and notice these recommendations
@Patrick_Ryan - let me change the question from what is a disease to - what is “Health”. WHO’s constitution pre amble is
By that definition - a person with disease may still be “Healthy”. The goal of medical profession is to help person achieve the state of “well-being”.
Now - lets visit your question - when does a disease end. It ends when the person has achieved the state of well-being.
We don’t observe “well being” in our data. We observe presence of/treatment for disease.
So - it is fair to say that
then i would say that the person although still has the chronic disease - has reached the best state of well being with respect to hypertension (i.e. well controlled or normotensive) - and is now in good health.
Maybe that signals the cohort end date! So how do we operationalize this in our data
This is ofcourse an opinion - and we have to test this. Cohort end date is a complex topic - but an important one for us all to tackle.
The atlas-phenotype.ohdsi.org has many such examples of cohort end date
See for example the Bronchitis cohort definition ATLAS
See the use of event -persistence. All Bronchitis events within the window are collapsed and 14 days offset
Using the concept set expression - i like to build cohorts that i expect would have variable sensitivity and specificity for the phenotype
| Id | Name | Estimated sensitivity | Estimated specificity |
|---|---|---|---|
| 135 | [Phenotype Phebruary][HTN] Essential Hypertension exclude secondary causes | *** | *** |
| 136 | [Phenotype Phebruary][HTN] Essential Hypertension no exclusions | **** | ** |
| 138 | [Phenotype Phebruary][HTN] Hypertensive disorder not limited to essential | ***** | * |
Now i am running Cohort Diagnostics - and will come back in a few hours to review results
May I suggest that we incorporate the populational scope of observational research? I totally agree that the anchor point for phenotype development is the clinical definition, but those are definitions that are meant to be used to identify individual patients during one or a series of related healthcare encounters. For populations ascertainment for research purposes, the definitions must be based on the clinical presentation but considering its operationalization at the populational level. For example, asthma is defined in a doctor’s office by means of anamnesis, family history, occupational history, bronchial challenge tests, lung function parameters, etc, etc. One of the most impacting findings of the historic ECRHS cohort studies, was to find out that there was a lot of undiagnosed persons with asthma in Europe (subclinical presentations, lack of awareness, etc) and that was possible because ECRHS developed and validated simple “phenotypes” based on symptoms that allowed higher sensitivity at the population level. Still those “phenotypes” were hardly transferrable back to the GP offices, but the message of increasing asthma awareness did. This situation of how different a clinical definition is (or needs to be) implemented in a populational study or in a doctor’s office can be applied to many other conditions starting with kidney diseases such as AKI or CKD.
@david_vizcaya i think it is reasonable to build phenotype definitions that use signs/symptoms. In the case of this phenotype, hypertension,
people most commonly should NOT have signs/symptoms that are directly attributable to hypertension e.g. hypertensive crisis may present with headache/blurry vision. presence of hypertensive crisis would exclude persons from the phenotype (in this case)