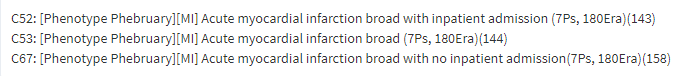
Evaluation of phenotypes for Acute Myocardial Infarction
Insights on sensitivity errors:
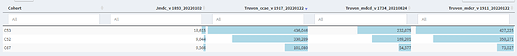
- Cohort count diagnostic:
- Data sources without capture of inpatient care introduces missing data problem with sensitivity errors. This does not mean inpatient should be part of the cohort definition. It means that if we do a study on myocardial infarction in a data source with no inpatient capture - we may potentially miss about 50% of persons who had acute myocardial infarction. In datasources with inpatient visit data - inpatient concept was present in more than 50% suggesting substantial difference by cohort definition in same data source. About 20% of persons appear to be have MI without an inpatient stay. The rate is higher in JMDC compared to US datasources indicating a lower specificity in JMDC. Inference do not use datasources that do not capture inpatient data for this phenotype.
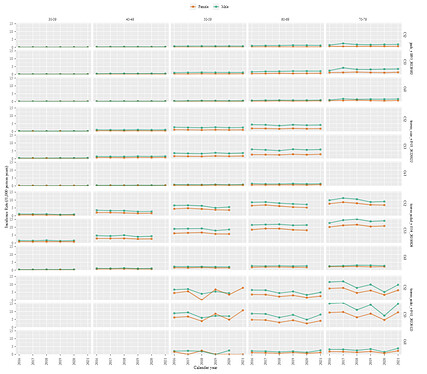
- Incidence Rate - Notice: for this diagnostic i tend to remove extremes of age and strata’s that have low counts (< 50)
- Incidence rate diagnostics shows temporal stability in the age strata with higher cohort proportion. Inference all the cohort definitions are temporally stable.
- Incidence rate is higher among Males compared to Females in most strata. Inference This is in line with clinical description.
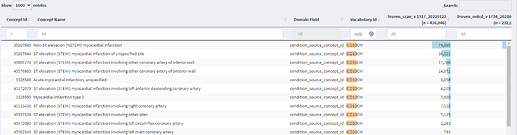
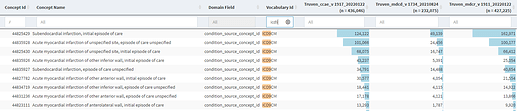
- Index event breakdown
- Few codes account for majority of the persons entry criteria and vast majority have low or zero counts. This shows that we are less likely to have sensitivity errors because of missing codes. Inference: orphaned codes are less likely to impact sensitivity.
- Index Event Breakdown shows that when filtering to ICD10CM - usage of cods for NSTEMI/STEMI
but filtering to ICD9CM does not have NSTEMI/STEMI
Inference studies that need the NSTEMI/STEMI classification of MI maybe limited to 2016 onwards - Non US datasource does not have NSTEM/STEMI codes, except CPRD Inference Although NSTEM/STEMI/ACS reflects contemporary definitions of Acute Myocardial Infarction - its not captured in source codes in many regions in the world.
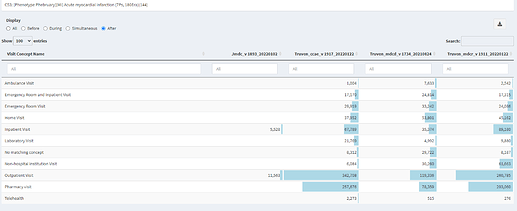
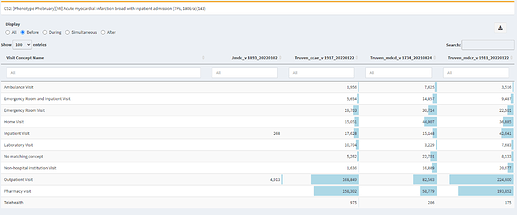
- Visit Context
- Inpatient visit is the most common visit that starts simultaneous with the cohort start date.
- Majority of persons in the cohort had an outpatient visit in the 30days after cohort start date. Inference persons experienced an event on index date that was associated with a subsequent care in the short term future (< 30 days)
- Majority of the persons were NOT experiencing an inpatient visit or ER visit in the period immediately prior to cohort start date. Inference: This suggests that in majority of persons the event of acute myocardial infarction is not part of a ongoing care episode - but potentially an event that started after an apparent period when no active care was sought.
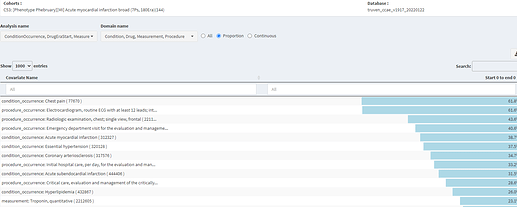
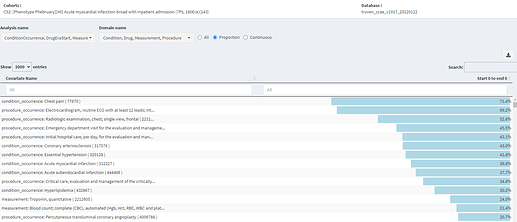
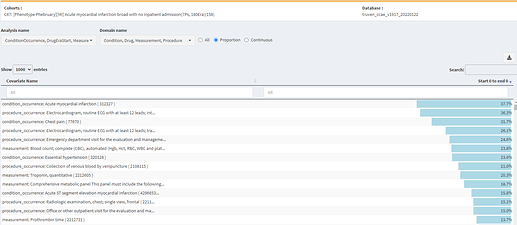
- Cohort Characterization:
- The vast majority of persons are coded with covariates expected to occur on Day 0 - Inference cohort definitions have good specificity.
- These covariate are higher for the cohort definition that requires inpatient admission - indicating that the specificity increases
compare to lower specificity for the cohort that does not include inpatient admission
Inference: This suggests that when we limit to persons who receive inpatient stay because that increases specificity. The loss in sensitivity may be upto 30% - Covariates on day 0 - that are observed in atleast 10% of persons include EKG, stress test/imaging. Inference These covariates may be used to improve the specificity in a cohort definition that does not require inpatient stay. Build a cohort of persons who have myocardial infarction but do not have the following covariates on index date. This cohort may be expected to have lowest sensitivity. Research idea: Can we build a rubric to identify covariates that when present/not present change the performance characteristics of cohort.
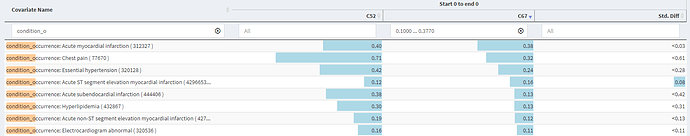
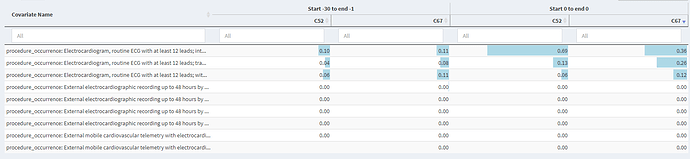
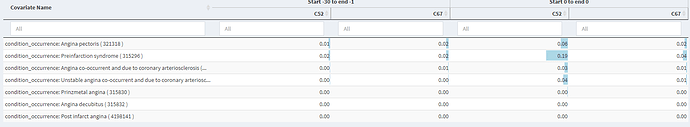
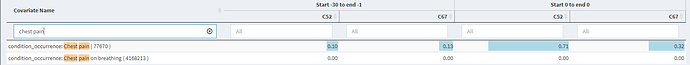
- Below we see covariates that are related to myocardial infarction in the period immediately prior to index date. We observe the rates to be low for EKG and Angina related concepts. Even the broad chest pain concept has a rate of up to 10% inference suggesting the upper limit of index date misclassification to be less than 10%, but in reality its much lower.
Use of EKG
Angina
Chest Pain
Next steps:
- Consider for persons who are not admitted to the hospital with a diagnosis of acute myocardial infarction - requiring that they have markers of severe disease such as EKG and chest pain.