Phenotype submission: Vasculitis without Phlebitis
Cohort Definition Name: “Vasculitis without Phlebiitis”
Contributor name: Jill Hardin
Contributor OrcId: 0000-0003-2682-2187
*Logic Descripton:*all occurrences of Vasculitis without Phlebiitis and no occurrences of skin infection’, starting between 90 days before and 0 days before cohort entry start date
Recommended study application: outcome, indication
Assertion statement: This cohort definition was executed on five real person-level observational health data source and resulted in a cohort with at least 1 person.
Submitted cohort definition:
VasculitisNoPhlebitis.txt (95.0 KB)
Target Clinical Description
Overview: Vasculitis is a comprehensive term used to describe a group of autoimmune disorders characterized by inflammation of the blood vessels. It is defined as the inflammation of blood vessels, including arteries, veins, and capillaries, resulting in tissue damage and compromised blood flow. Vasculitis can affect various organs and tissues throughout the body, leading to a wide range of clinical manifestations. As described by the Mayo Clinic, “Vasculitis involves inflammation of the blood vessels. The inflammation can cause the walls of the blood vessels to thicken, which reduces the width of the passageway through the vessel. If blood flow is restricted, it can result in organ and tissue damage. There are many types of vasculitis, and most of them are rare. Vasculitis might affect just one organ, or several. The condition can be short term or long lasting. Vasculitis can affect anyone, though some types are more common among certain age groups.”1 There are many different types of vasculitis including central nervous system vasculitis, cutaneous vasculitis, Kawasaki disease, Microscopic polyangiitis, Cogan’ Syndrome, Behcet’s disease, Buerger disease, Churg-strauss syndrome, Takayasu’s arteritis, cryoglobulinemia, giant cell arteritis, granulomatosis with polyangiitis, and Henoch-Schonlein purpura.1,2
Presentation: Typical signs, symptoms, or defining patient features of vasculitis include: Cutaneous manifestations: These include skin rashes, petechiae, purpura (small purple spots), or ulcers. Constitutional symptoms: Fever, fatigue, weight loss, or night sweats. Joint pain, swelling, or stiffness. Neurological symptoms: Peripheral neuropathy, mononeuritis multiplex, or central nervous system involvement, depending on the specific form of vasculitis. Organ-specific symptoms: Respiratory symptoms (cough, shortness of breath), kidney dysfunction, gastrointestinal symptoms, eye redness or pain, or oral ulcers. According to the Mayo Clinic and or the Cleveland Clinic, common symptoms of vasculitis may include fever, fatigue, aches/pains including joint pain, skin rashes, headache, vision changes, and weight loss.1,2 Depending on the part of the body, other symptoms may develop as well. For example, if the lungs are affected by vasculitis one may experience shortness of breath.1
Diagnostics Evaluation: Evaluation for vasculitis may include a physical exam, blood tests, urinalysis, a pathergy test, ultrasound or other imaging tests (e.g., CT, MRI, PET scan, chest X-ray), fluorescein retinal angiography, or biopsy.1,3
Therapy Plan: The therapy plan may include management of the cause or underlying condition, corticosteroids, anti-inflammatory medicine (e.g., non-steroidal anti-inflammatory medicines [NSAIDs]), intravenous immunoglobulin (IVIG), other mediations, or procedures such as plasmapheresis.1,4
Prognosis: The short-term clinical outcome for a patient with vasculitis within 3 months post-diagnosis can vary depending on the specific subtype and the severity of the disease. Acute treatment response, the presence of complications, and underlying comorbidities can also influence short-term prognosis. The long-term clinical outcome for patients with vasculitis, observed over a year or more, is diverse and highly dependent on various factors. These factors include the specific subtype of vasculitis, the presence of underlying systemic diseases, response to treatment, and adherence to management strategies. Long-term prognosis can range from relatively good outcomes in certain forms of vasculitis with appropriate treatment to a more chronic and progressive course in other cases, especially if complications or multiorgan involvement are present.
References:
-
Mayo Clinic. Vasculitis. Vasculitis - Symptoms and causes - Mayo Clinic.
-
Cleveland Clinic. Vasculitis. Vasculitis | Cleveland Clinic.
-
NIH National Heart L, and Blood Institute Vasculitis Diagnosis. Vasculitis - Diagnosis | NHLBI, NIH.
-
NIH NH, Lung, and Blood Institute. Vasculitis treatment. Vasculitis - Treatment | NHLBI, NIH.
-
Suresh E. Diagnostic approach to patients with suspected vasculitis. Postgrad Med J. 2006;82(970):483-488.
Logical Description:
Cohort Entry Events
People may enter the cohort when observing any of the following:
condition occurrences of vasculitis without phlebitis.
Inclusion Criteria
No skin infection (SNOMED concept id 4029043 and all descendants) starting between 90 days before and 0 days before cohort entry start date.
Cohort Exit
The cohort end date will be offset from index event’s start date plus 365 days.
Interpretations:
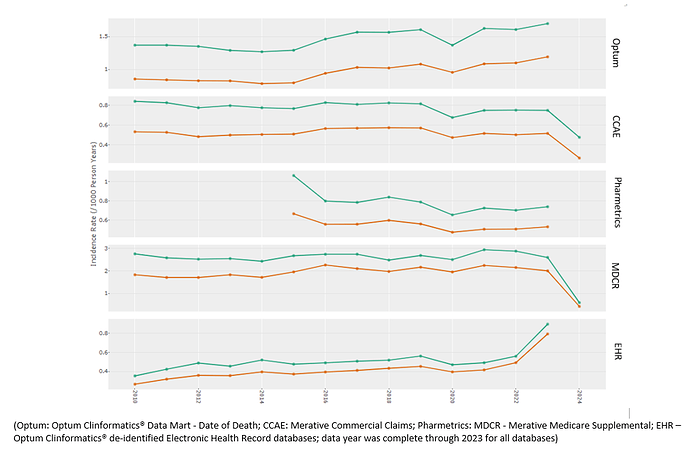
The final concept set expression had 178 concepts for vasculitis without phlebitis from the condition (n=173) and observation (n=5) domains, respectively. Identification of vasculitis without phlebitis ranged from 101,000 cases in Merative Medicare to 361,000 in Optum Clinformatics® DOD. Between 22% (IQVIA Pharmetrics) to 35% (Merative MarketScan® CCAE) of subjects had the code for “arteritis” (standard concept code: 314659), and between 11% (Merative CCAE) to 39% (Merative MarketScan®Medicare) had the code “temporal arteritis” (standard concept code: 4290976). The annual incidence rate estimates among subjects were stable across the databases (Figure 1). Rates were ~ 3 times higher in ages > 50 years compared to ages < 50 years. Rates were ~30% higher in females compared to males.
Figure 1. Incidence rate pattern over time generated by Cohort Diagnostics
green = female; orange = male
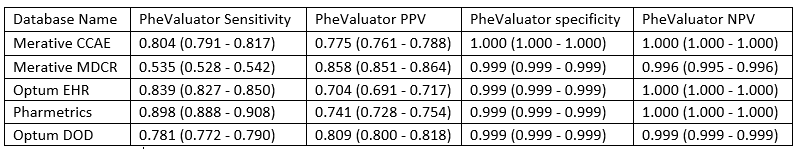
Summary of PheValuator reported operating characteristics.
The PheValuator tool estimated the mean sensitivity of the phenotype to be 77% and the mean positive predictive value to be 77% across the databases.
Summary of phenotype performance metrics estimated via PheValuator tool
Literature Review:
LitReview vasculitis and malignancy.docx (31.0 KB)
Recommendations:
Please come visit our poster at OHDSI Global Symposium 2024