Hi, @Dymshyts et al!
I’m really sorry that we’ve been keeping all these CPT4 concepts in the Standard area for that long, so the change cost became that big.
Nice to hear it, Dima!
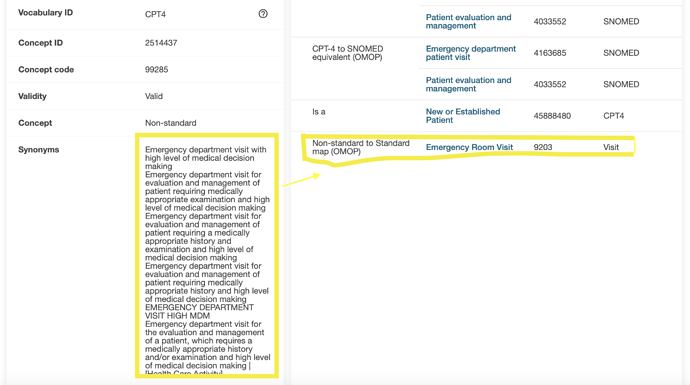
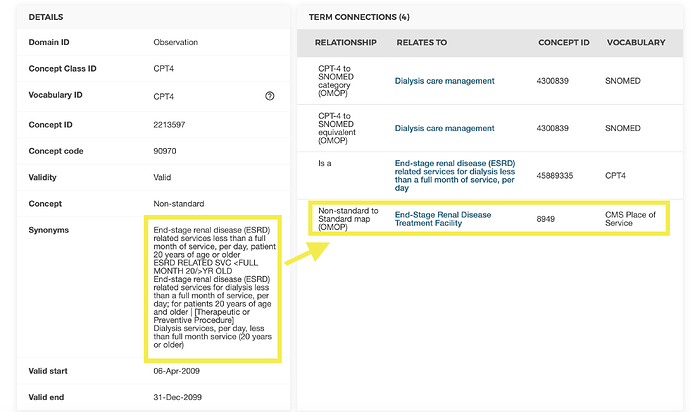
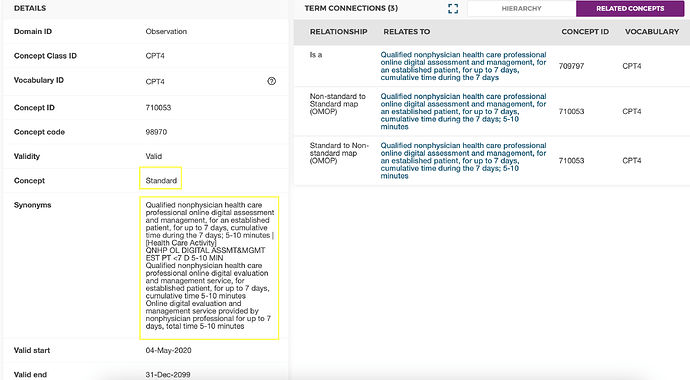
The problem lies much more on the surface: these codes have highly variable meanings even within a code. And how the given user interprets them depends on many factors including the specific knowledge of the vocabulary and coding rules, locally established practices, and the ability for mental gymnastics with multiple AND/OR statements and logical reasoning.
Users can’t do that. We don’t want users to do that. And this is not what the Standard concepts are supposed to be.
We keep working on the vocabulary improvement project and we’ll release vocabulary principles later this year (link1, link2). In line with the principles we keep improving the vocabulary cleanliness, and this case (among others, like negative information, Survey data) is one of the most characteristic examples to look at.
But right, if users find this information useful, we need to find a proper solution to Standardize it.
How about the following?
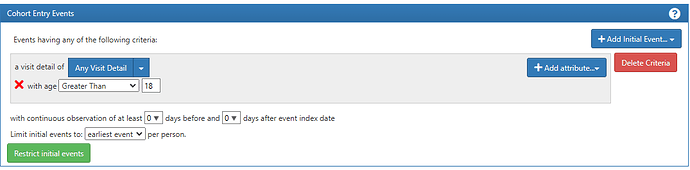
- We ask folks who know and use CPT4/HCPCS in research to boil them down and extract meaningful information from them. Not the entire CPT4/HCPCS pool - only those that don’t qualify the criteria for Standard concepts (those mapped to Visits and other deStandardized concepts). Dima already started this work by identifying those that are used in cohorts or otherwise characterize the patients.
- We look at the meaningful information together and decide what the proper Domains should be. Could be the Visit, Observation, Modifier? or something else.
- Then we find a way to record this information in the proper Domain, or make an exclusion. The solution could trigger the creation of new more specific concepts within the existing hierarchies of Visit, or the Visits of new dimensions, or new Observation concepts in the OMOP Extension.
- We come up with a guide for ETL, including the approach for merging the Visits coming from different sources, if needed.
- Since CPT4/HCPCS is on the roadmap the vocabulary team can help with 3, 2, and partially 4, but we still need your help with 1 and 4.
- In the meantime, given that the problem has persisted for more than 1.5 years (4 latest vocabulary releases) and the release cycle is 6 months, we try to focus on the solution space to get a proper approach implemented by the nearest release in August as opposed to make a rollback/shortcut solution in the nearest release and postpone the proper solution for the future.
Thoughts?