Phenotype submission: Parasomnia
Cohort Definition Name: “Parasomnia”
Contributor name: Gowtham A Rao
Contributor OrcId: 0000-0002-4949-7236
Logic Descripton: First occurrence of Parasomnia.
Recommended study application: outcome, indication
Assertion statement: This cohort definition was executed on atleast one real person-level observational health data source and resulted in a cohort with at least 1 person.
Submitted cohort definition: Parasomnia.txt (4.7 KB)
Target Clinical Description
Parasomnia may be defined as a category of sleep disorders characterized by abnormal movements, behaviors, emotions, perceptions, and dreams that occur while falling asleep, sleeping, between sleep stages, or during arousal from sleep. The defining features of Parasomnia often include: Motor Activity (Involuntary complex movements), Vocalization (Verbal outbursts, such as moaning, screaming, or even talking can manifest), Altered Consciousness (impaired cognition and diminished awareness during the episode, distinguishing it from other sleep disorders in that daytime sleepiness is usually not affected). Some of the common synonyms include Somnambulism (sleepwalking), Night Terrors, REM Behavior Disorder, Confusional Arousal. The diagnosis is often clinical but may be assisted by Polysomnography and some standardized questionnaires. Treatments include cognitive behavioral therapy. Use of pharmacotherapy is controversial. The prognosis is variable or unknown; it may be transient or may persist long-term. Differential diagnosis would include sleep apnea, restless leg syndrome, seizure disorders, narcolepsy. Co-morbid conditions may include insomnia, anxiety disorders, depression and chronic pain conditions. In general a person who also has epileptic seizures (mutually exclusive) it makes the diagnosis of Parasomnia less likely but they may co-occur.
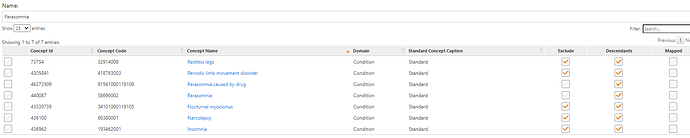
Specifically - in our shared clinical understanding of Parasomnia as documented in the clinical description above, we decided to not include restless leg syndrome, periodic limb movement, narcolepsy, myoclonus, insomnia in our entry event criteria. We think that these clinical condition may very well co-occur in the person, but they are not by themselves sufficient to make a person eligible to be part of Parasomnia cohort.
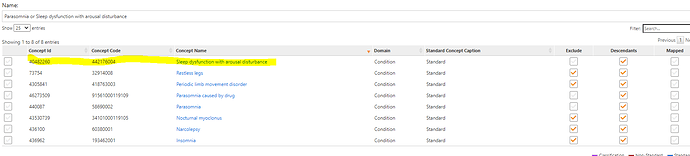
Building concept set.
Build Initial Concept Set
We started with initial SNOMED concept 73754 Parasomnia. This SNOMED codes descendants include concepts below that based on target as described above did not meet the entry criteria. i.e. a person may have these codes at the same time (co-occur), but the codes are not considered sufficient to allow a person to enter into the cohort.
- 73754 Restless legs
- 4305841 Periodic limb movement disorder
- 43530739 Nocturnal myoclonus
- 436100 Narcolepsy
- 37397765 Insomnia co-occurrent and due to nocturnal myoclonus
We created the initial concept set as follows.
Mapping analysis
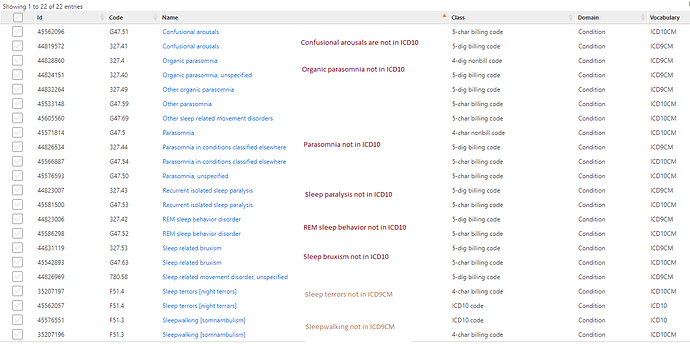
We looked at the mapped non-standard concepts (e.g. ICD codes). We observed the following:
Difference between ICD10/ICD10CM and ICD/ICD9:
Observations
- ICD10 introduced codes for Sleep terror disorders & sleep walking. They did not exist in ICD9CM.
- ICD9CM had codes for Organic parasomia. These were dropped in ICD10.
- ICD10CM introduced codes that were not in ICD9CM or ICD10.
- ICD10CM has concepts representing bruxism, sleep paralysis, Parasomnia, confusional arousal.
- ICD10CM builds on top of ICD9CM with sleep terror disorders and sleep walking. Note: sleep terror and walking are in ICD10.
Questions that come to mind:
- How were persons with night terrors or Somnambulism coded in ICD9CM?
- How are persons with bruxism, sleep paralysis, Parasomnia, confusional arousals identified in non ICD9CM/ICD10CM codes.
Impact on cohort definitions.
Anecdotal opinion: we expect this cohort definition to have sensitivity, specificity and index date misclassification errors because of the nature of the disease itself. Most individuals may not seek care or when they seek care they likely are misdiagnosed, and the diagnosis may take some time. Many of these errors may not be observable in our observational data.
However, the following potential errors are empirically observed:
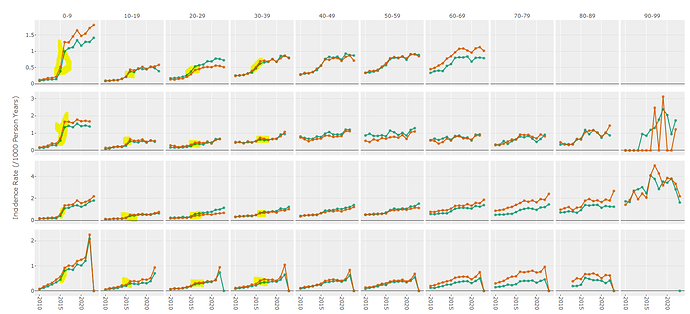
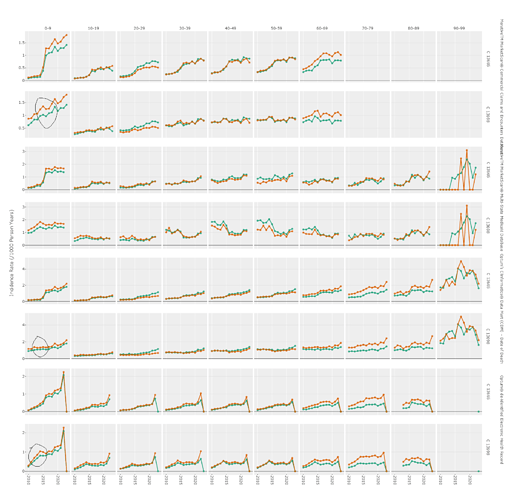
A) Sensitivity errors:
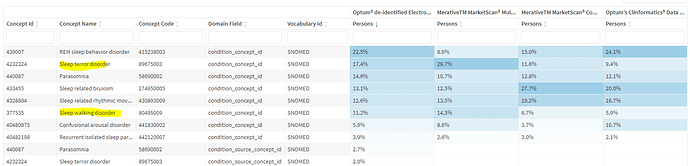
- In US data sources, prior to 2016 there is a dramatic shift. This is explained by introduction of night terror/sleep walking codes, that appear to account for up to about 50% of persons post 2015. (2015/October/1 was the date ICD10CM was introduced).
- In non US data sources that rely on ICD10 vocabulary, the age distribution and baseline characteristics are different. ie. the persons identified to have Parasomnia in ICD10CM has higher proportion of adults and polysomnography, while those in ICD10 vocabulary data sources were almost exclusively children less than 10 years. The population level characteristics of persons identified in ICD10CM with the codes not in ICD10, appear to be consistent with profile of patients with Parasomnia. This suggests there is sensitivity errors in ICD10 data sources, i.e. ICD10 data sources are only able to identify persons with sleep terrors and sleep walking.
B) Specificity errors:
We see some evidence that a persons may have either gotten an additional diagnosis of a differential condition in the future after their diagnosis of Parasomnia. As described in the clinical description, it is possible for some of the differential to co-occur in a person with Parasomnia - but it may also represent a revision of diagnosis. The temporal characterization diagnostics in cohort diagnostics, shows occurrence of diagnosis listed in differential diagnosis in time periods after index date such as Restless leg (about 5%)/Obstructive sleep apnea (33% in the 1 year after). The high rates of Obstructive
sleep apnea may suggest specificity errors.
3) Index date misspecification:
We observe > 10% of individuals to have diagnosis of obstructive sleep apnea or insomnia prior to first Parasomnia diagnosis. If these persons truly had Parasomnia, then it may be possible that the first date they were diagnosed with either obstructive sleep apnea or insomnia should be the corrected date of Parasomnia.
Recommendations:
- Overall - this definition has errors that may need to be quantified using methods like PheValuator.
- How to overcome the sensitivity errors in ICD9CM:
- we suggest limiting studies to period that starts on or after 2017-01-01. This gives about 1 year post ICD10CM implementation for data to accrue using ICD10CM. This acrual period in 2016 calendar year may allow us to differentiate between persons who had pre-existing condition vs new onset Parasomnia.
- the other strategy is to identify if alternate codes were used in ICD9CM to identify persons with Night terrors, or sleep walking.
- we suggest not to study Parasomnia in data sources that are using ICD10 vocabulary because the vocabulary is lacking the granularity to capture clinical ideas like bruxism, sleep paralysis, Parasomnia, confusional arousal that appear to represent 50% of cohort in ICD10CM based data sources.
- How to overcome specificity errors:
- we dont have recommendations to improve specificity without compromsing sensitivity. Some ideas to explore are use of sleep study or counselling or behavioral therapy. The later care is less likely to be documented systematically in observational data and thus restricting may increase sensitivity errors.
- Index date specificity errors:
- we dont have recommendations for index date misspecification corrections. Options maybe to index on visits for sleep related disorder if they were within 1year prior to when a person may enter the cohort based on codes in Parasomnia concept set.