Previous OHDSI work:
Assigned Peer reviewer:
@Evan_Minty
Neutropenia
Authoritative source
Summary from authoritative source:
Overview
Defects in neutrophil function can be quantitative, as seen in neutropenia or qualitative, as seen in neutrophil dysfunction. This phenotype is quantitative decrease in neutrophils. Neutropenia is ANC <1500 cells/microL in an adult while agranulocytosis is a more severe form of neutropenia with ANC <200 cells/microL. Acute is < 3 months. Agranulocytosis is part of neutropenia. Note: pancytopenia may include Neutropenia.
Neutrophils play a role in the immune defense against extracellular bacteria, including Staphylococci, Streptococci, and Escherichia coli, among others. They also protect against fungal infections, including those produced by Candida albicans. Once their count is below 1 x 10/L recurrent infections start. Neutropenia that is found in association with sepsis, hemodynamic instability, respiratory compromise, fever, or other clinical emergencies - require immediate hospitalization and urgent evaluation.
Neutropenia, with decreased production with marrow hypoplasia, can be primary and due to chronic benign neutropenia, cyclical neutropenia, and other congenital and familial neutropenias. It can be secondary to cytotoxic drugs, aplastic anemia, leukemia, drug reactions, and infections. Neutropenia, with increased destruction with marrow hyperplasia, is due to hypersplenism and immune neutropenia. Secondary causes are the commonest. Congenital forms are rare and vary in severity – including leukocyte adhesion deficiency, Chediak-Higashi syndrome, hyper-IgE, recurrent infection syndrome, and chronic granulomatous disease.
Presentation
- The neutropenia is often asymptomatic or presents with an insidious onset. history of recurrent infections, infections by rare bacteria and fungi, opportunistic infections with observation of low to absent absolute neutrophil count
- The clinical presentation is usually oral ulcerations with or without fever, but occasionally sepsis may be the initial presentation. Fever, mouth sores, or gingival disease inflammation.
- Timing to exposure (drug) when direct or indirect toxicity is the operative mechanism: the presentation may be delayed for months. Most cases of severe neutropenia or agranulocytosis present within the first six months and usually within the first three months after beginning the offending drug. Unlikely to occur immediately after inciting agent, Vancomycin-induced neutropenia indicated that most cases occurred after a minimum of seven days of treatment, with the majority occurring at least 20 days after initiation of treatment. Rechallenge requires both a latent period and high drug doses before recurrence is observed. Rechallenge, or inadvertent subsequent administration, is associated with a prompt recurrence even with low doses.
Assessments:
Immunoglobulin assays, microbiological studies
Plan:
Find and treat/prevent exposure to offending agent. Granulocyte-colony stimulating factor (G-CSF) may be used, especially when recurrent infections is occurring. Use of antimicrobials as prophylactic and treatment of infections. Allogenic bone marrow transplantation from an HLA-matched related donor can cure CGD.
Prognosis:
- Can the person fully recover marking the end of an episode i.e., is full recovery possible, or is it considered life long? Can fully recover
- If it’s not lifelong and recovery/end of condition is possible – on median
- What is the minimum (median) duration that persons are expected to have the disease? Any neutropenia longer than 2 months is considered chronic neutropenia. So, a good median estimate for all cause neutropenia maybe 3 weeks (21 days)
- What is the maximum (median) duration that persons are expected to have the condition? Congenital, ethnic, and hereditary neutropenias may be life-long. We can estimate the median to be 365 days.
- If end of condition is possible, can a new episode of the condition independently re-occur in the same person after full recovery from prior independent episode? Yes
Strengtheners:
Drugs known to cause neutropenia include - Quinidine, Aminopyrine, Cephalosporin, Sulfonamides, Hydralazine, Penicillin’s, Heavy metals, Phenothiazine.
Antineutrophil or autoimmune neutropenia has been observed in: Rheumatoid arthritis (Felty syndrome), Inflammatory bowel disease, Chronic autoimmune hepatitis, Granulomatosis with polyangiitis, Hodgkin lymphoma, Sjogren syndrome
Bone marrow biopsy may indicate a suspicion towards bone marrow etiology.
Underlying autoimmune disease, like rheumatoid arthritis and SLE, Viral infections like hepatitis, HIV and EBV, HPV reactivation, Nutritional deficiency (e.g., copper or vitamin B12 deficiency), Treatment with granulocyte colony-stimulating factor, Symptoms: oral ulcers, fever, sepsis, gingival disease
Disqualifiers:
- Normal neutrophil count or elevated neutrophil count Concurrent/<7 days before (because cannot occur overnight)
- Familial/congenital neutropenia, benign ethnic neutropenia all time
- Bone marrow transplant all time
Designated Medical Event - MedDRA PT terms:
Granulocytopenia
Has neutropenia as a component: Aplastic anaemia, Bone marrow failure, Pancytopenia; Neutropenic colitis, Neutropenic infection, Neutropenic sepsis
Notes from phenotype development:
Terms Neutropenia vs Leukopenia: [Decision] Since Neutrophils are the major component of white blood cells (~75%) and the occurrence of having normal neutrophil counts in the presence of low white blood cell count is rare – we decided to consider granulocytopenia and leukopenia as synonyms. However, we decided to not consider the terms lymphocytopenia, eosinopenia as synonyms for neutropenia – as they clearly represent granulocytes that are not neutrophils.
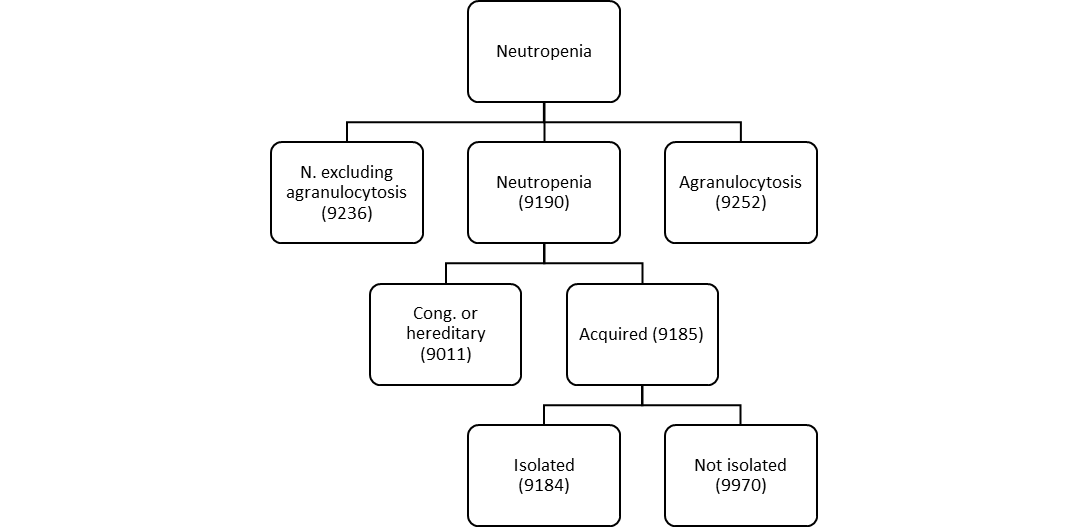
Degree of neutropenia: [Decision] Patients degree of severity of neutropenia correlates with their risk of infection. Severe reduction of neutrophils is agranulocytosis. Degree has implications on patient’s outcome. So, we decided to attempt three different variations of Neutropenia (Neutropenia, Agranulocytosis, Neutropenia without agranulocytosis).
Use of laboratory results in cohort definitions: [Decision] We decided to use the American Board Of Internal Medicine 2022 laboratory test reference range in the definition, which are as follows: Absolute neutrophil count (ANC) – 2000–8250/μL, 2000 to 8250/microL, 2 to 8.25 x 10/L (SI); Leukocyte count 4000 to 11,000/microL, 4.5 to 11 x 109/L (SI); Segmented neutrophils: 50 to 70 percent. Agranulocytosis < 200.
Congenital or Hereditary Neutropenia vs Acquired Neutropenia: [Decision] Persons with neutropenia may have neutropenia because of congenital or genetic conditions. Those persons cannot have acquired neutropenia. We decided to define Acquired Neutropenia as those persons who do not have a diagnosis of congenital or acquired neutropenia.
Single cell line vs Multiple cell lines: [Decision] Neutropenia may be part of multiple cell line penia’s like pancytopenia’s related to peripheral destruction or (more commonly) bone marrow failure/aplastic anemia. We decided that persons with neutropenia limited to one cell line where a different phenotype compared to persons who had neutropenia that was part of multiple cell lines involvement. We decided to define the persons with single cell line involvement as isolated neutropenia. We expect the persons with isolated neutropenia to be rarer than pancytopenia.
Data quality: [Decision] We observed that in rare occasions for a person to have a lab result corresponding to neutropenia, while another lab result on the same day is in the normal range. We decided that these may represent FALSE positives, potentially due to lab errors – and decided to remove those individuals.
Notes from phenotype evaluation:
Pending
Submission checklist: Discussed here
- Forum post (started)
- Clinical Description (complete)
- Literature Review (pending)
- Logic Description (complete)
- Recommended cohort definitions (>= 1) (complete)
- Published cohort diagnostics output (pending)
- Discussion of evaluation (pending)
- CohortDefinitionSet (pending)
Shiny application