Diabetic ketoacidosis
Cohort Definition Names
- Diabetic ketoacidosis IP-ER (SNOMED concept)
- Diabetic ketoacidosis IP-ER (SNOMED concept + lexical recommendations)
- Diabetic ketoacidosis IP-ER w concurrent insulin (SNOMED concept)
- Diabetic ketoacidosis IP-ER w concurrent insulin (SNOMED concept + lexical recommendations)
Logic descriptions
• All condition occurrences of DKA during an ER or IP visit, with 30-day event persistence (SNOMED code only)
• All condition occurrences of DKA during an ER or IP visit, with 30-day event persistence (SNOMED + lexical recommendations)
• All condition occurrences of DKA, during an ER or IP visit with overlapping insulin exposure (SNOMED code only)
• All condition occurrences of DKA, during an ER or IP visit with insulin exposure between 0-14d relative to DKA (SNOMED code only)
Only Cohort #1 json included: diabetic ketoacidosis IP-ER (SNOMED concept).txt (3.8 KB), although all were evaluated.
Contributor names
Clinical description
Overview
Diabetic ketoacidosis (DKA) is a potentially life-threatening complication of diabetes mellitus, an extreme metabolic state caused by absolute insulin deficiency or relative insulin deficiency, which occurs more frequently in patients with T1DM (Misra 2015). Because the body does not have enough insulin to allow sugar into the body’s cells for use as energy, the liver breaks down fat for fuel. The breakdown of fatty acids (lipolysis) produces ketone bodies (ketogenesis), which are acidic. Acidosis occurs when ketone levels exceed the body’s physiological management capacity. DKA is characterized by the triad of hyperglycemia, anion gap metabolic acidosis, and ketonemia.
Presentation
DKA is an urgent clinical situation, which evolves quickly, sometimes within 24 hours. The common symptoms may include nausea and vomiting, pronounced thirst, excessive urination, feeling weak or fatigue, short of breath, fruity-scented breath, maybe confused, and abdominal pain that may be severe. Weight loss may be associated with the dehydration. Polyuria, polydipsia, and weight loss may often persist for several days before hospital admission. Signs of volume depletion such as decreased skin turgor, dry axillae and oral mucosa, low jugular venous pressure, tachycardia, and, if severe, hypotension. Deep respirations reflecting the compensatory hyperventilation (called Kussmaul respirations) Lab test may show high blood sugar level and large amounts of ketones in blood and urine. In some cases, they may be presented as euglycaemic DKA (blood sugar ~< 11mmol/L or 200 mg/dL).
Obesity and a family history may be associated with an increased risk of DKA. It can also be triggered by mismanaged insulin dose, physical or emotional trauma, severe acute illness (e.g., MI, stroke, pancreatitis), pregnancy, drug abuse (e.g., cocaine) surgical procedures, dehydration, extensive exercise, surgery, low-carbohydrate diets, excessive alcohol intake, or certain medicines (e.g., corticosteroids and some diuretics).
Assessment
Physical examination may identify signs and symptoms associated with DKA and medical history evaluation would identify the underlying disease of diabetes and may also discover other causes that have led to DKA episode, e.g., infection, preparation or undergoing surgical procedures, or inadequate insulin administration. The eventual clinical diagnosis of DKA may arrive when the combination of hyperglycemia (high blood sugars), ketones in the blood or on urinalysis and acidosis are demonstrated (Chiasson 2003). Lab testing may include elevated anion gap metabolic acidosis caused by the accumulation of beta-hydroxybutyric and acetoacetic acids. Most patients are mildly hyponatremic (low sodium) on presentation. There are acute elevations in the BUN and serum creatinine concentration, which reflect the reduction in glomerular filtration rate induced by hypovolemia. In about 10% of cases the blood sugar is not significantly elevated (“euglycemic diabetic ketoacidosis”) (Abbas 2009).
The American Diabetes Association categorizes DKA in adults into one of three stages of severity (Abbas 2009):
- Mild: blood pH mildly decreased to between 7.25 and 7.30 (normal 7.35–7.45); serum bicarbonate decreased to 15–18 mmol/L (normal above 20); the person is alert
- Moderate: pH 7.00–7.25, bicarbonate 10–15, mild drowsiness may be present
- Severe: pH below 7.00, bicarbonate below 10, stupor or coma may occur
Treatment plan
DKA needs to be treated either in the emergency room (ER) or admitted to the hospital. Treatment usually involves:
- Fluid replacement: Fluids replace those lost through too much urinating. They also thin out the blood sugar. Fluids can be given by mouth (mild ketoacidosis or dehydration) or through intravenous (IV) fluids to achieve quick fluids replacement.
- Electrolyte replacement: Electrolytes are minerals in the blood, such as sodium, potassium and chloride, that carry an electric charge. IV electrolytes are given to help keep the heart, muscles and nerve cells functioning properly.
- Insulin therapy: Insulin reverses diabetic ketoacidosis. In addition to fluids and electrolytes, insulin is given, usually through a vein. A return to regular insulin therapy may be possible when the blood sugar level falls to about 200 mg/dL (11.1 mmol/L) and the blood is no longer acidic.
Prognosis
DKA is a serious complication that requires immediate clinical care in the ER or admitted to the hospital. The condition could be effectively managed with fluid replacement, electrolyte replacement, and insulin therapy. In severe cases (e.g., cerebral edema and coma) with delayed clinical care, the condition can be associated with increased risk of mortality.
References
- Misra S, Oliver NS. Diabetic ketoacidosis in adults. BMJ. 2015 Oct 28;351:h5660. doi: 10.1136/bmj.h5660. Erratum in: BMJ. 2015;351:h5866. PMID: 26510442.
- Chiasson JL, Aris-Jilwan N, Bélanger R, Bertrand S, Beauregard H, Ekoé JM, Fournier H, Havrankova J. Diagnosis and treatment of diabetic ketoacidosis and the hyperglycemic hyperosmolar state. CMAJ. 2003 Apr 1;168(7):859-66. Erratum in: CMAJ. 2003 May 13;168(10):1241. PMID: 12668546; PMCID: PMC151994.
- Abbas E. Kitabchi, Guillermo E. Umpierrez, John M. Miles, Joseph N. Fisher; Hyperglycemic Crises in Adult Patients With Diabetes. Diabetes Care 1 July 2009; 32 (7): 1335–1343.
Phenotype development
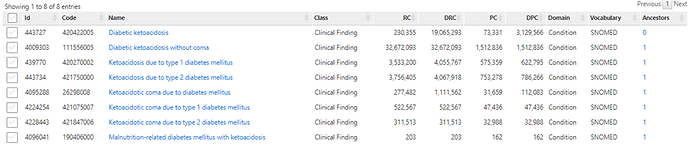
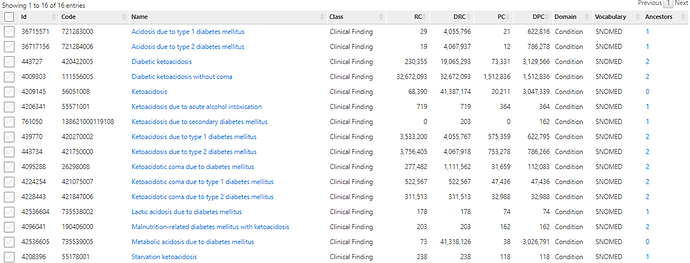
Concept set development
-
Initial concept set: Diabetic ketoacidosis SNOMED clinical finding concept (443727) + descendants
-
Second concept set: Diabetic ketoacidosis SNOMED clinical finding concept (443727) + lexical recommendations
Cohort logic development
First, we defined the 2 cohorts defined by condition occurrences in the inpatient or emergency department setting. Following discussion with clinical colleagues, we defined 2 additional cohorts that required insulin exposure temporally proximal to the DKA diagnosis, despite our awareness that inpatient drug exposures are poorly captured in US insurance claims databases.
Study applications
We included 30-day event persistence when calculating incidence proportion during a 21-day time-at-risk, so that we wouldn’t observe multiple events per time-at-risk period per patient.
Phenotype evaluation
Cohort Diagnostics
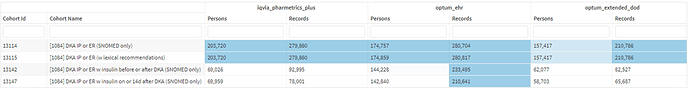
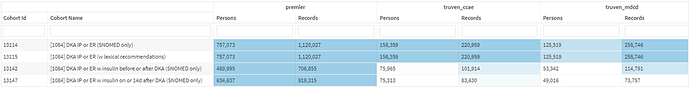
Diagnostics were executed against 7 databases: 5 US administrative claims databases, 1 US electronic health records database, and 1 US hospital database.
Cohort counts
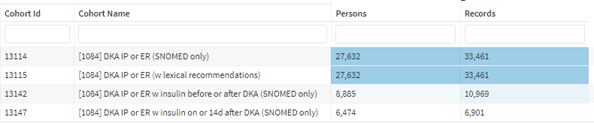
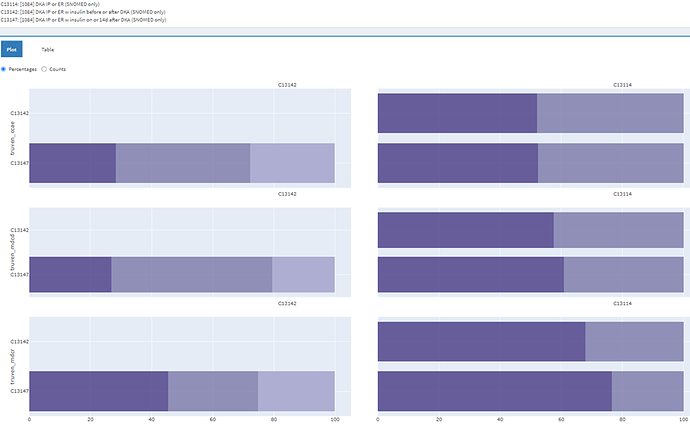
Cohorts 13114 and 13115, that differ only in terms of the addition of lexical concept recommendations in cohort 13115 return the same number of patients and events in all US claims data sources and Premier. The patient and event counts differ trivially in Optum EHR. As expected in US claims data, there is a considerable drop in event and patient counts when we restrict to patients with concurrent insulin exposure (Cohorts 13142 and 13147). There is a less substantial, but still non-trivial patient count reduction when this restriction is applied to Optum EHR and Premier.
Cohort overlap
The identical counts observed in cohorts 13114 and 13115 were confirmed to be the same patients in the cohort overlap diagnostic. For the remaining overlap we will only assess Cohort 13114. In IBM US claims data, cohort 13114 (DKA IP/ER SNOMED only) overlapped with insulin-restricted cohorts by ~50% in CCAE, ~60% in MDCD, and ~70% in MDCR. In IBM US claims, cohort 1342 (DKA w overlapping insulin) overlapped with cohort 13147 (DKA with insulin 0-14d) by ~30-50%. In remaining databases, cohort 13114 (DKA IP/ER SNOMED only) overlapped with insulin restricted cohorts by ~20% in Optum EHR, ~60% in Optum DOD, and ~70% in PharMetrics. In these sources, cohort 1342 (DKA w overlapping insulin) overlapped with cohort 13147 (DKA with insulin 0-14d) by ~40-90%.
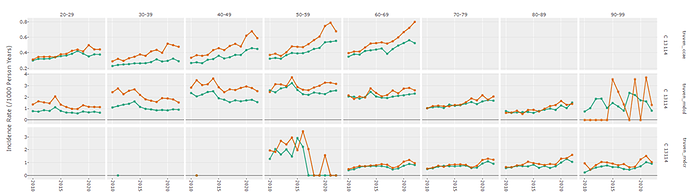
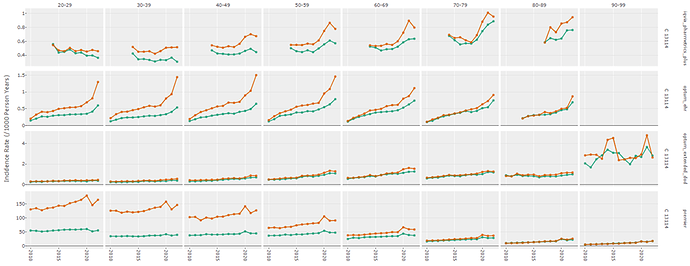
Incidence rates
For cohort 13114 (DKA IP/ER SNOMED only), the 3 IBM US claims database show that background DKA rates are higher among men than women, which is contrary to some reports (Adult Diabetic Ketoacidosis - StatPearls - NCBI Bookshelf). There is an increase over time on CCAE. Counts among older patients in MDCD (>90 years) and younger patients in MDCR (<60 years) are few rendering the rates unstable and difficult to interpret. The magnitude of the background rates (range 0.3-1.0/1k person-years) which is at the low end of what is reported in literature (0-56/1k person-years) (Adult Diabetic Ketoacidosis - StatPearls - NCBI Bookshelf). Rates for the definitions restricted to insulin use were all low in these databases because inpatient dispensing records are poorly recorded in US claims data.
Cohort 13114 (DKA IP/ER SNOMED only) show some similar trends in PharMetrics, Optum DOD, Optum EHR, and Premier. The background DKA rates are higher in men than women and increase over time most notably in Optum EHR. The magnitude of the observed rates is considerably lower than those reported elsewhere except in Premier, an all-inpatient database, where rates range from 4-180/1k person-years. It should be noted that observation time is limited in premier so rates may be inflated by virtue of smaller denominators. Among DKA patients restricted to those with insulin use, we observed similar trends, including higher rates in males, rates increasing over time, and substantially higher rates in Premier than the other sources. There is little indication that DKA event rates substantially drop from 2014 to 2015 which would suggest ICD9CM to ICD10CM code mapping to SNOMED needs investigation.
Characterization
Potential sensitivity errors (failure to include patients we want)
Are expected clinical events absent from characterization results?
Are clinical events of lower prevalence than expected given what we know about the phenotype?
Per the clinical description, “DKA is characterized by the triad of hyperglycemia, anion gap metabolic acidosis, and ketonemia”
Hyperglycemia lower than expected. We observed 20-30% temporally proximal to index, although we expected 100%.
Ketonemia was not observed, but this condition is rarely observed in all internal databases. To observe this in a DKA would probably be redundant with observing DKA.
Increased anion gap was expected in all DKA cases, and we observed “Metabolic acidosis, increased anion gap (IAG)” at 100% prevalence. This is encouraging.
Low sensitivity metrics calculated via PheValuator suggest more sensitivity errors may be present (See Validation section).
Potential specificity errors (failure to exclude patients we do not want)
Are unexpected clinical events present in characterization results?
Are clinical events of higher prevalence than expected given what we know about the phenotype?
Differential diagnoses per Adult Diabetic Ketoacidosis - StatPearls - NCBI Bookshelf
-
Hyperosmolar hyperglycemic nonketotic syndrome
*Hyperosmolarity 0-3%, hyperglycemic disorder 0-2% on index - Starvation ketosis
*0% on index -
Myocardial infarction
*7-10% on index -
Pancreatitis
*~5% on index -
Alcoholic ketoacidosis
*0% on index, but various alcohol-related conditions observed -
Lactic acidosis
*0% but elevated level of transaminase and lactic acid dehydrogenase ~1% -
Sepsis
*8-16 % on index -
Toxicologic exposure
*ethylene glycol 0% on index
*methanol 0% on index
*paraldehyde 0% on index
*salicylate 0% on index -
Diabetic medication overdose
*uncaptured -
Uremia
*0% on index
The main conditions that could indicate non-trivial specificity errors are myocardial infarction (7-10% on index) and sepsis (8-16% on index). It is unclear from the observational data if these diagnoses indicate true conditions occurring concurrently with DKA, or if they represent possible alternative diagnoses instead of DKA. Specificity metrics calculated via PheValuator are all >99% (See Validation section).
Potential index date misclassification (failure to accurately identify disease onset)
Are clinical events indicative of disease onset observed before phenotype index date?
No conditions, drugs, or procedures indicative of DKA observed in the [-30 to -1d] window relative to index indicating that the DKA clinical event could have occurred before the diagnosis was recorded. This may be consistent with the acute and IP/ER nature of DKA presentation.
Characterization results per content in clinical description
-
Presentation (index):
*Nausea and vomiting (15-20%), fatigue (5-10%), abdominal pain (12-20%), dehydration (24-29%), Polyuria (~1%), polydipsia (0%), tachycardia (10-20%), hypotension (0%), insulin (20-45%), severe acute illness (e.g., MI, stroke, pancreatitis) (<5%), pregnancy related findings (~1%), alcohol and substance abuse (2-10%), infections (6-10%), hypovolemia (2-9%), urinalysis (8-30%) -
Treatment plan (index, 1-30d):
*Fluid replacement (unobserved)
*Electrolyte replacement (75-78% Optum EHR, 10-15% in other sources - inpatient drug exposures poorly captured in claims)
*Sodium, sodium chloride (~70% Optum EHR, 6-12% in other sources - inpatient drug exposures poorly captured in claims)
*Potassium (alone and in combination with antihyperglycemics ~50% in Optum EHR, lower in other sources)
*Insulin (~30-80% in Optum EHR, lower in other sources)
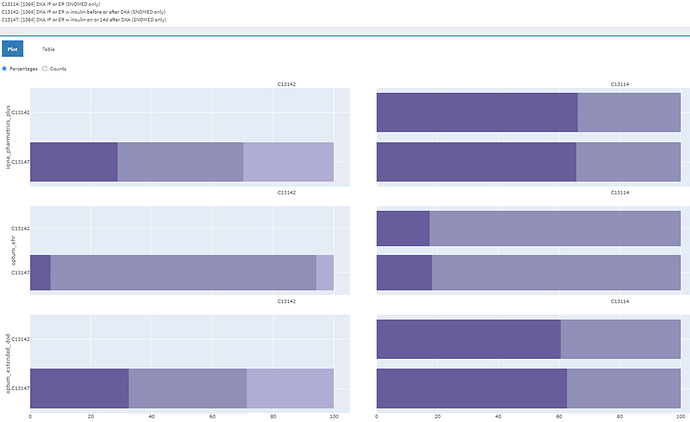
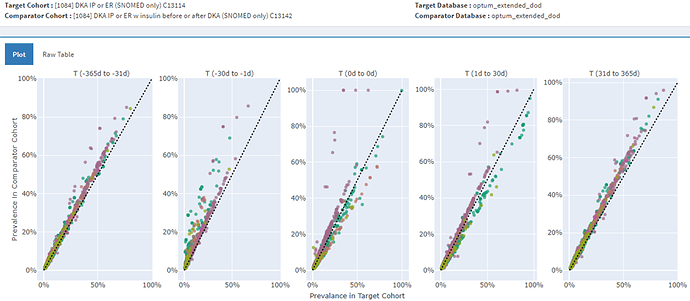
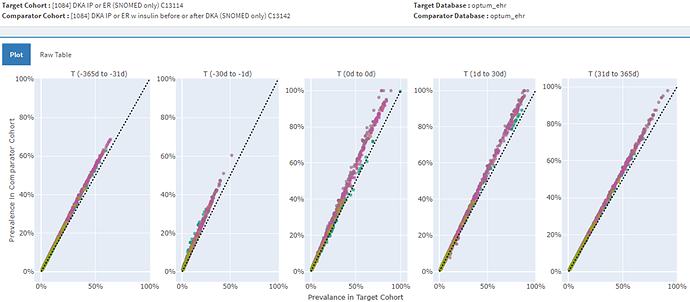
Comparative characterization
Cohorts 13114 (DKA IP/ER SNOMED only) and 11315 (DKA IP/ER SNOMED w lexical recommendations) have complete patient overlap so characterization comparison showed identical covariate distributions.
Comparing cohort 13114 (DKA IP/ER SNOMED only) with cohort 13147 (DKA IP/ER 0-14d insulin) in US claims sources with poor IP drug dispending capture showed greater prevalence of clinical events in cohort 13147 before and after the index DKA event (including greater insulin exposure on and after index, per the definition).
Comparing cohort 13114 (DKA IP/ER SNOMED only) with cohort 13147 (DKA IP/ER 0-14d insulin) in Optum EHR with better IP drug dispensing data showed greater prevalence of clinical events in cohort 13147 (DKA IP/ER 0-14d insulin), but with fewer unstable, high prevalence insulin covariates on and after index.
Validation
We used probabilistic reference standard-based validation (PheValuator) to calculate measurement error metrics for our candidate phenotype definitions.
The full PheValuator results are in the embedded file:
diabetic ketoacidosis IP-ER (SNOMED concept) PV summary.xlsx (12.6 KB)
Sensitivity, specificity, and PPV minimum and maximum values are included in the table below. For all definitions, sensitivity was lowest in MDCR and was highest in Optum EHR. For all definitions, specificity was lowest in MDCD and was highest in CCAE when not restricted to insulin users in CCAE, and highest in PharMetrics when restricted to insulin users. Error metrics between cohorts 13114 and 13115 were identical because these two definitions returned the same patients. Restrictions requiring insulin therapy (13142 and 13147) decrease sensitivity and increase specificity and PPV. Optum EHR results may show the high sensitivity because of availability of inpatient drug exposure data in this source, which may better specify the diagnostic predictive model.
| Cohort ID | Description | Sens min | Sens max | Spec min | Spec max | PPV min | PPV max |
|---|---|---|---|---|---|---|---|
| 13114 | DKA IP-ER SNOMED only | 0.266408 (MDCR) | 0.720846 (Optum EHR) | 0.996845 (MDCD) | 0.999492 (CCAE) | 0.51412 (MDCR) | 0.791607 (Optum EHR) |
| 13115 | DKA IP-ER SNOMED w lexical recos | 0.266408 (MDCR) | 0.720846 (Optum EHR) | 0.996845 (MDCD) | 0.999492 (CCAE) | 0.51412 (MDCR) | 0.791607 (Optum EHR) |
| 13142 | DKA IP-ER overlapping insulin | 0.126362 (MDCR) | 0.654933 (Optum EHR) | 0.99949 (MDCD) | 0.999928 (PharMetrics) | 0.685579 (MDCR) | 0.865025 (PharMetrics) |
| 13147 | DKA IP-ER 0-14d insulin | 0.096529 (MDCR) | 0.652794 (Optum EHR) | 0.999595 (MDCD) | 0.999936 (PharMetrics) | 0.723577 (MDCR) | 0.875383 (PharMetrics) |
Recommendation
Given the patient count reduction when applying concurrent insulin restrictions in US claims data sources and characteristic differences between cohorts with vs without insulin exposure restrictions, we recommend Cohort 13114 (DKA IP/ER SNOMED only) as the phenotype that returns patients most representative of the clinical description. Generally low sensitivity and PPV values in certain databases should be noted if using this phenotype definition in certain data sources.