Thank you @Christian_Reich for volunteering to perform an evaluation on the candidate cohort definitions for Acute Hepatic Failure. Your evaluation is due on February 8th 2023.
Briefly - we are aiming to phenotype Acute Hepatic (liver) Failure. According to EASL (EASL Clinical Practical Guidelines on the management of acute (fulminant) liver failure - PubMed), Acute Liver Failure (ALF) refers to a highly specific and rare syndrome, characterized by an acute abnormality of liver blood tests in an individual without underlying chronic liver disease (such as cirrhosis).
To perform the evaluation, @Christian_Reich will be provided the following:
- Clinical description (see below)
- Cohort definitions
- Output of Cohort Diagnostics available at data.ohdsi.org/PhenotypeLibrary
Clinical Description:
Acute hepatic failure refers to the development of severe acute liver injury with encephalopathy in a patient without cirrhosis or preexisting chronic liver disease. Clinically, the presence of encephalopathy is the key differentiator of acute hepatic failure from other forms of liver injury, i.e., the mere presence of coagulopathy, impaired liver synthetic function or liver injury in the absence of encephalopathy is not considered acute hepatic failure. Encephalopathy may vary from altered mental status to coma. Symptoms include fatigue/malaise, lethargy, anorexia, nausea and/or vomiting, right upper quadrant pain, pruritus, jaundice, and abdominal distension. Signs on physical exam may include orthostatic hypotension, coagulopathy, vesicular skin changes, ascites, right upper quadrant tenderness, jaundice, and hepatomegaly. Common assessments include liver enzymes, bilirubin, coagulation/INR/ prothrombin time (PT), hepatitis viral serology. Look for Acetaminophen exposure. The condition is managed in specialized center, hospitals with liver transplant program. N-acetylcysteine is used for the treatment of acetaminophen toxicity. Supportive care includes bleeding prevention, infection prevention, nutritional support, monitoring for ammonia levels, encephalopathy, hypoglycemia, hypokalemia, hypomagnesemia, and hypophosphatemia. Prognosis depends on severity/underlying causes and need for liver transplantation. An episode of acute liver failure may be considered to have ended if person is discharged from hospital, receives liver transplantation, ceases to have encephalopathy.
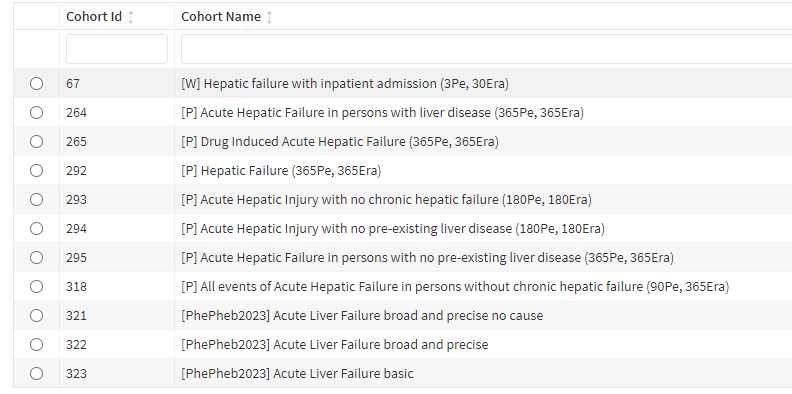
Cohort Definitions:
- Cohort Id 67: Hepatic Failure with inpatient.
- Logic description: Persons with hepatic failure, necrosis, encephalopathy or comma and managed in a inpatient or emergency setting.
-
Cohort Id 292: Hepatic Failure. Logic description: Persons with hepatic failure or encephalopathy, but not chronic hepatic failure.
- Logic description: Persons with hepatic failure or encephalopathy, that do not also have chronic hepatic failure. This exclusion to because according to EASL definition persons with prior liver disease are not considered eligible to have acute hepatic failure.
-
Cohort id 295: Acute Hepatic Failure in persons with no pre-existing liver disease. Logic description: Persons with hepatic failure but not Chronic Hepatic Failure and many other liver related diseases.
- Logic description: Persons with hepatic failure or encephalopathy that do not also have chronic hepatic failure and other liver diseases including Viral Hepatitis, Liver Cirrhosis, Liver Fibrosis, Toxic Liver Disease, Hepatic Necrosis, Alcohol use disorder, Alcoholic Hepatitis, Alcoholic ,Fatty Liver, Malignancies that spread to liver (breast, esophageal, stomach, pancreatic, lung, kidney, melanoma), Chronic Hepatic Failure, Other Chronic Liver Disease, Ascites, Portal Hypertension, History of Liver Transplant, Cholestasis, Non-Alcoholic Fatty Liver Disease, Autoimmune Hepatitis, Primary Biliary Cholangitis.
Output of Cohort Diagnostics: for the above cohort are available at data.ohdsi.org/PhenotypeLibrary .