Posting on behalf of @AzzaShoaibi
(the forum does not allow new users to post images or links!)
Team:
Day 9 of Phenotype Phebruary. I happen to be the bravest to pick a date for my phenotype that ends
Patrick amazing dense posts and start an era of “OK” Phenotype Phebruary posts. I hope that you will still find my input useful!
Today, I’ll try to start a conversation of the phenotype that came to us during phenotype development and evaluation workgroup office hours. Our friend Aize wanted to know how can we phenotype delirium in observational data. Together we started the process of 1. Decide on the clinical description of delirium 2. Accumulate prior knowledge on the phenotype 3. Select initial concept set (codes)-using phoebe and Atlas. Those 3 steps took place during last week office hour. I then took the action of completing the next steps of 4. Build one or more cohort definition using atlas 5. Evaluate and iterate on the definition using cohort diagnostics. I will summaries my learnings today to Aize and you all, hoping that this will start a useful discussion
Clinical description:
My favorite paper that summarized what delirium is and what we know about it is here: Burns, A., Gallagley, A., & Byrne, J. (2004). Delirium. Journal of Neurology, Neurosurgery & Psychiatry , 75 (3), 362-367, but here is a quick overview of some points that I found relevant to the phenotyping exercise.
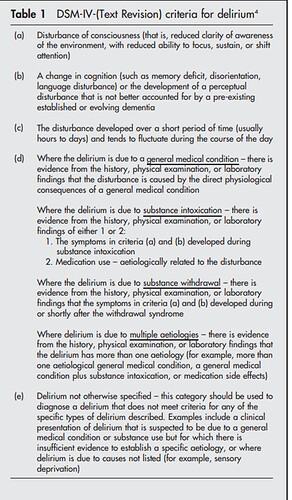
Delirium, or a confused mental state, occurs suddenly. A person has a change in mental status and acts disoriented and distracted. Delirium is more common in older adults, especially those with dementia, and people who need hospitalization. Prompt treatment is essential in helping a person with delirium recover. Delirium happens when a person has sudden confusion or a sudden change in mental status. The person may have trouble paying attention or thinking clearly. They may act disoriented or distracted. Delirium is more severe than having a “senior moment” — the minor problems people have with memory and understanding as they get older. It requires treatment and often hospitalization. Delirium is not a disease, It’s a changed mental state. Because delirium is temporary, it’s hard to know exactly how many people develop it. Researchers estimate that hospital delirium affects 15% to 50% of people. Below is the exact clinical criteria for delirium by DSM-IV to guide our way
You will notice above that the clinical description includes all “kinds” of delirium and is NOT limited to delirium due one reason or another for example: delirium due to “general medical condition”.
Phenotype development:
If you had the superpowers to go through Patrick’s Phenotype Phebruary posts from day1-8, you would know by now that there are 2 ways to start phenotype development. 1. Start de novo and use OHDSI tools to search the vocabulary, to build your initial concept set and decide on a logic for your initial cohort definition (using the clinical description and other clinical material as the main guide) or 2. Replicate published literature. I like to take the 2 approaches at the same time. I will try to demonstrate how I did that with delirium.
I started with my best friend PHOEBE. The tool recommended the standard concept “delirium”– no surprises here- as the initial concept. I then pasted all included concept IDs of “delirium and it’s decedent” into PHOEBE concepts set recommender. PHOEBE (did not crash ![]() and identified the following missing code/clinical ideas:
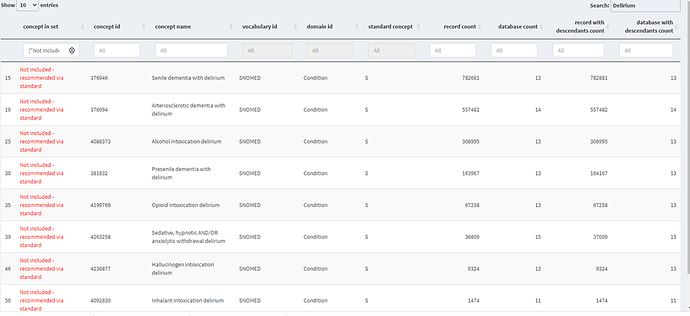
and identified the following missing code/clinical ideas:
Senile dementia with delirium, Arteriosclerotic dementia with delirium, Alcohol intoxication delirium, Presenile dementia with delirium, Opioid intoxication delirium, Sedative, hypnotic AND/OR anxiolytic withdrawal delirium, Hallucinogen intoxication delirium and Inhalant intoxication delirium are all clinical ideas that are within the scope of the clinical description above. So, it made sense to add them to the definition. It is worth mentioning that those codes were recommended by both “standard” and “sources” codes (Thank you Phoebe).
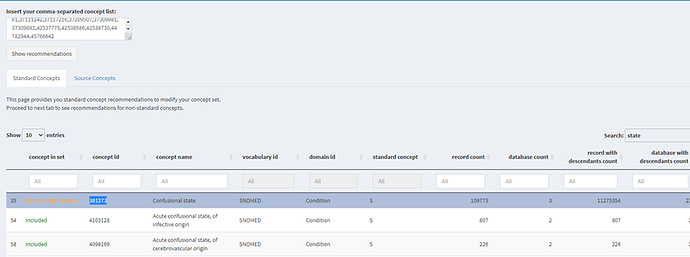
Phoebe also recommended the standard code “Confessional state” going by semantics “Confessional state” is actually a synonym to delirium, however the clinical criteria include additional requirements. I did a quick search to explore the utility of this code across our data.
Confessional state is basically the parent of delirium in the SNOMED hierarchy. Pheobe already tells me that there are 109,773 records loaded on this code across OHDSI network. However, it does not map to any source code used in any of the data sources I have access to- including ICD10CM, ICD10, ICD9CM, READ, etc). This practically means that if I to use it in the definition it won’t have any implication on any of the data sources, I have access to. However,” Confessional state” might be needed to capture cases of delirium in other data sources where (for clinical or coding practice reasons) more generic codes tend to be used and hence the recode count observed in PHOEBE.
Finally, I did a quick search and looked at included source codes in Atlas and confirmed that my concept set covers all source vocabularies that I am familiar with. At that point I felt good about my concept set and I am ready to build a cohort (or more). To build a cohort (in atlas or in any other way) we need answer the following questions:
What event(s) let you enter the cohort?
What inclusion criteria are applied to those events?
For each event, how long do you satisfy the inclusion criteria?
How should events be combined into cohort eras?
Let’s start to answer these questions to build one or more delirium cohort definition. I know that 99.9% of you will argue that one needs to know exact analytical use of the cohort definition (the research question at which the definition will be used for) to answer these questions correctly. Indeed, most would argue that even selecting concept sets should be based on the exact analytical use or research question. This is how I like to think: the phenotype development should be primary based on the clinical description of the phenomena we are trying to model (the target) ; taking into consideration the general context of the research that it will be used for. Updating the cohort definition to fit a certain/specific use can always be done at a later stage.
What event(s) let you enter a delirium cohort?
To answer this question, I will remind you of few facts from the clinical description: “Delirium is more severe than having a “senior moment” — the minor problems people have with memory and understanding as they get older. It requires treatment and often hospitalization”. “Delirium happens more often in older people and hospitalized patients. “Hospital delirium” can affect 10% to 30% of those patients”.
During office hours, we asked Aize about the context at which she needs the phenotype for, she told us that it is for research investigating rates of delirium among hospitalized covid patients.
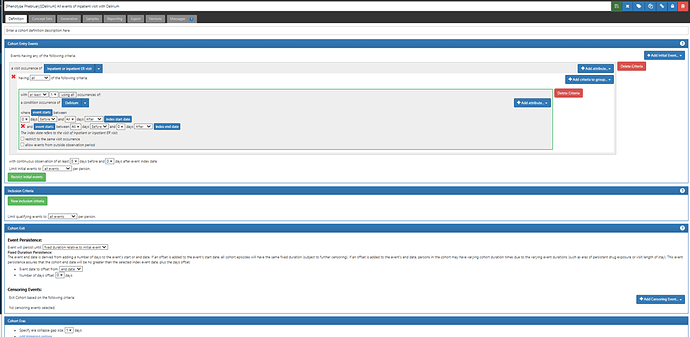
Given the clinical description, what we know about delirium and the research context, an inpatient hospital visit may be the appropriate entry criteria for the cohort. In which case, one can argue that “hospitalized delirium” is a more accurate target here- totally agree.
What inclusion criteria are applied to those events?
If the entry event is the hospital visit, then an inclusion criterion should be an occurrence of a delirium diagnosis during the hospital stay (i.e an occurrence of a delirium diagnosis the overlaps with the time duration between hospital start and hospital ends)
For each event, how long do you satisfy the inclusion criteria?
We learned from the clinical description that “Delirium is not a disease, it’s a changed mental state and is temporary”. So there should be a point in time that delirium is resolved (patients exit the cohort) and have the chance to develop Delirium again as an independent episode or event (re-enter the cohort). Looking at clinical papers I quickly found that duration of delirium is (7 days ± 7days). However, given that the start of hospital stay is the index I chose for the cohort, then end of hospital stay is a logical end date for the cohort. This means every hospitalization with an overlapping occurrence of delirium diagnosis will be considered one event/episode of delirium and patients are allowed to have more than one event if these events occur in different in-patient visit.
How should events be combined into cohort eras?
@Patrick_Ryan demonstrated how we should think about cohort eras carefully through the kidney stone phenotype. In the delirium case, we have less of a problem in this definition since we are using a hospital visit as the indication of the event. But one might ask, if someone is discharged from a hospital stay during which delirium was diagnosed/recorded and was then readmitted in the same day (possibly to another hospital) with delirium; would you consider that a true new event. To solve this possible edge case, I chose to use an era collapse gap size to be 1 day.
The full implementation of this cohort definition in Atlas can be found here: ATLAS (for those with access to the phenotype development Atlas)
So now I have 1 definition that I came up with de novo, time to look at what others have done! .
Cohort definition from literature :
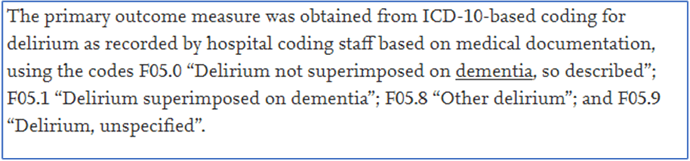
A quick literature search on possible existing phenotypes for delirium revealed that most prior research (that I found) took a simple approach and defined the disease using the main /few ICD10 cm codes, example below. I happily confirmed that all these codes are already subsumed in my definition (a nice sanity check that Atlas allows you to do by going to source codes tab)
I then found a very interesting paper titled: “Enhancing Delirium Case Definitions in Electronic Health Records Using Clinical Free Text.” By McCoy et al. Enhancing Delirium Case Definitions in Electronic Health Records Using Clinical Free Text - ScienceDirect. In brief the author proposes different delirium alternative based on claims data (going from narrow to broad by adding an ICD9 generic code). They conclude that even when using the broadest definition, the rate of delirium observed is far lower than the current literature estimates.
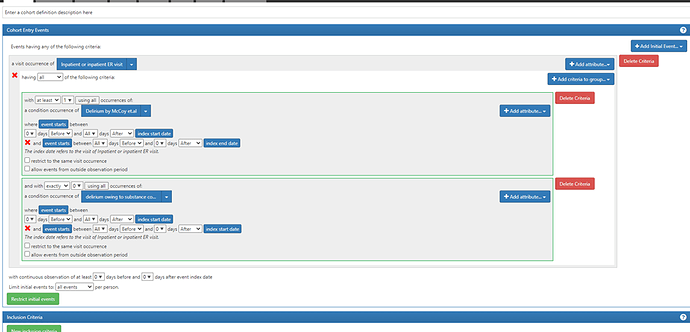
I found here that the narrow definition they propose is similar to the de novo definition I came up with (another nice sanity check). However, the broadest definition uses an extremely common ICD9- code (780.09 (“other alteration of consciousness”)) that will sure have a big impact. Based on that I decided to replicate their definition and add it to my cohorts to evaluate. The implementation of the McCoy et al cohort is here
https://atlas-phenotype.ohdsi.org/#/cohortdefinition/118
cohort evaluation:
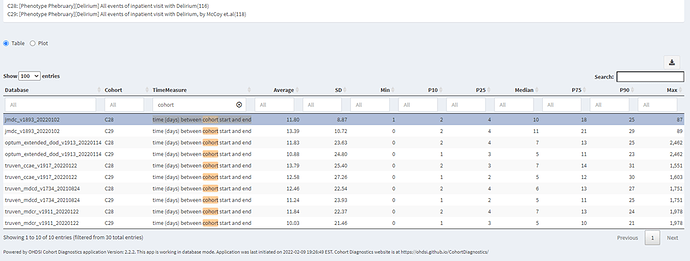
I’ll use CohortDiagnostics to start to evaluate the two cohorts above. The results are publicly available at:: https://data.ohdsi.org/phenotypePhebruary . as a reminder, the two cohorts are :
C28: [Phenotype Phebruary][Delirium] All events of inpatient visit with Delirium(116):
C29: [Phenotype Phebruary][Delirium] All events of inpatient visit with Delirium, by McCoy et.al(118): the cohort informed by the literature
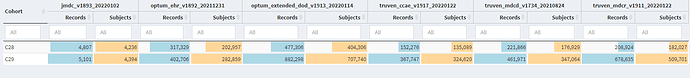
When we look at the Concept Counts, we can see that the additional code that McCoy et.al added “other alteration of consciousness”, has a substantial impact on the number of qualifying persons in each cohort. In CCAE/MDCD/MDCR, we see that the number of patients more than doubled.
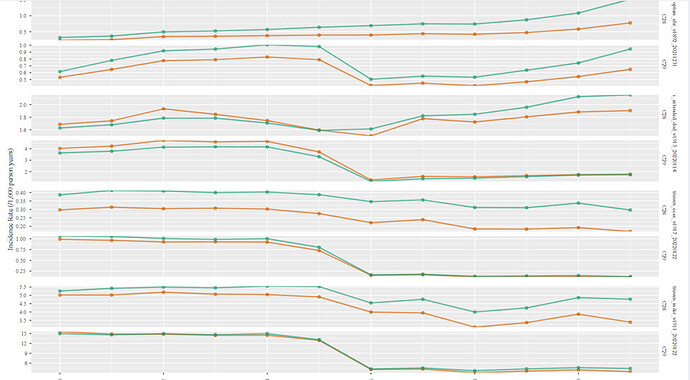
Now, let’s look at the Incidence Rate analysis:
While cohort C28 looks fairly stable over time, there is significant drop in incidence rate of McCoy et.al. across all US based data sources. This is explained by the fact that McCoy et.al added an icd9cm code to improve the sensitivity of the definition. While I deliberately used the mapped standard SNOMED code hoping that the standard vocabulary would allow the clinical idea to be captured across other vocabulary (ICD10cm,in this case) , it didn’t really work. Even if we believe that McCoy et.al. has a better sensitivity, the definition (as is) can’t be used post 2015 due to the transition to ICD10cm. an extra step and iteration will be needed.
Let’s look at time distribution, it’s interesting to check how our logic played out in the data, for both cohort the medium time (days) between cohort start and end ranged from 5 to 11 days. This is consistent with my clinical notes about delirium hospitalization.
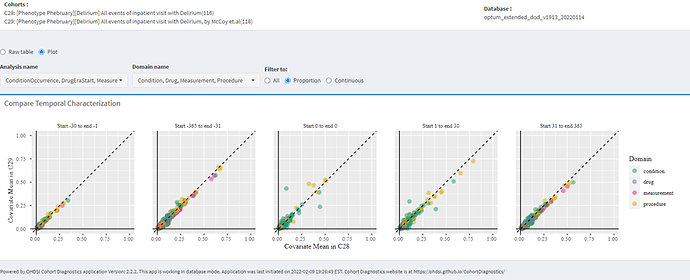
So, let’s turn to Temporal Characterizations to see if we can find any insights:
whenever I evaluate two cohorts where one is broader than the other, I like to quickly check the covariate distribution plot in cohort diagnostic. The question I am trying to answer here is “how similar/comparable are patients in the two cohorts" . If indeed the two cohorts had very similar covariate distribution (at baseline). that may suggest that they are the same type of people; now if one cohort has significantly more count than the other, then I would lean toward going with the broad definition because why would I exclude half the people (roughly in this case) when I have no evidence that they are different than those I am including.
In this case I can see some differences in the occurrence of some procedures and conditions.
Now the next step would be to go dig into temporal characterization to check for further insights
There are so much to see in cohort diagnostics but maybe this is enough to start the conversation! Encourage you all to look into CD and share you thoughts of what you see