In this post, we will focus on drug-induced liver injury (DILI) and adjudicating potential cases.
In short:
-
DILI is different from other conditions in the way that it is a) rare, b) condition of exclusion, с) has a potential causal relationship already embedded in the phenotype
-
In developing phenotype, we would optimize NPV rather than PPV; focus on defining the conditions of exclusion; maybe create several phenotypes to be used across the network since it’s not clear if one phenotype would fit every data source
-
Case adjudication for finding new associations needs some smart methods since it’s impossible to review thousands of patients
-
We lean towards trusting notes (unstructured data) more than a code for DILI in the structured data, but in fact inferring patient status is hard either way and is subjective.
-
Maybe, discontinuation of the drug after the liver injury can be a useful indicator but we need to figure out how to infer discontinuation reliably.
If that sounds interesting, read on.
DILI is a good example of a condition that perfectly fits observational research. Since it’s so rare, it is rarely captured in small size clinical trials, which points out the need for post-marketing research.
It used to be the most frequently cited reason for drug withdrawal (up to 32% of drug withdrawals, recently decreased following FDA statements). We know about an increased risk of DILI for some of the drugs (e.g., acetaminophen,amoxicillin-clavulanate, antiepileptics). There are many outdated stats regarding DILI prevalence and proportion in liver disorders, but what we know for sure is that it varies geographically and is more common in adults.
Presentation: can mimic both acute and chronic liver diseases, both hepatocellular and cholestatic. Can be symptomatic or only include asymptomatic liver test abnormalities. If symptoms are present, they include malaise, low-grade fever, anorexia, nausea, vomiting, right upper quadrant pain, jaundice, acholic stools, or dark urine.
Suspect when a patient has underlying liver conditions or has taken drugs that metabolize in liver.
Diagnosis:
- No other conditions of exclusion (such as autoimmune hepatitis, Wilson disease, viral hepatitis, ischemic liver injury, Budd-Chiari syndrome)
- Various hepatic lab tests (alkaline phosphatase >2 times the upper limit of normal + ALT/ALP ratio ≤2, bilirubin ≥2.5 mg/dL, etc.)
- Biopsy (optional)
Treatment: mainly drug discontinuation, sometimes glucocorticoids; for some of the drugs – antidotes (like N-acetylcysteine for acetaminophen and L-carnitine for valproic acid toxicity).
Prognosis depends on the severity and form of injury. In severe cases can progress to hepatic decompensation, encephalopathy etc.
Informatics approach:
Overall notes:
-
Drug induced liver injury is a rare condition and is mostly a disorder of exclusion meaning that all of the other cases have to be ruled out prior to establishing the diagnosis.
-
Given that we want to use the phenotype in safety surveillance, we are interested in a rather specific phenotype. NPV should be prioritized over PPV.
-
It would be nice if we could just take SNOMED 4144765 Drug-induced disorder of liver and be done with it. Of course, it doesn’t get used very often.
Therefore, we need to create a phenotype, which will have three elements:
-
a liver injury (diagnosis, symptom or lab test defined)
-
a drug exposure preceding liver injury (would be cool to use external knowledge to select the drugs that metabolize in liver @callahantiff)
-
no other causes (may get tricky if a patient has an underlying liver disorder that can be both the risk factor for DILI and an alternative diagnosis)
We decided not to reinvent the wheel and take the existing phenotype that eMERGE has previously developed (led by @hripcsa and @chunhua). Others exist, but that one has the most discussion about phenotype development, details on implementation and the same data source at our disposal. They’ve done huge work on developing and implementing the phenotype, which as you can imagine took some time (@hripcsa said ~ 6 months – I’m really surprised it took ONLY 6 months).
Link: https://academic.oup.com/jamia/article/20/e2/e243/710321?login=true#supplementary-data
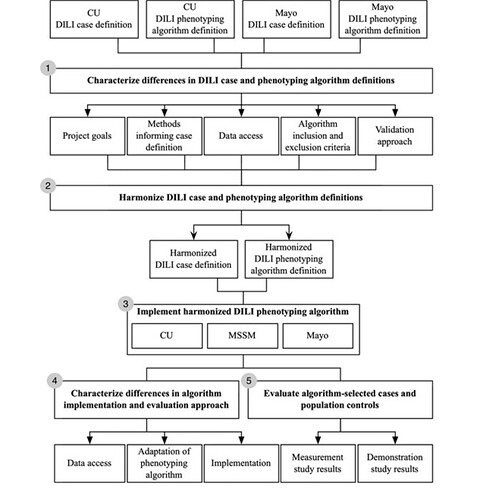
I’ll post a figure on phenotype development in eMERGE here as I find it quite interesting:
Basically, two institutions developed their algorithms which were then fused. Also, interesting how the gold standard was created there (intersection of the patients identified by the NLP algorithm and by the acute liver injury ICD-9 algorithm).
We borrowed a lot from their phenotypes (ATLAS):
-
- Patients aged 18
-
- Index date: any of the liver injury codes in the original implementation mapped to SNOMED + PHOEBE-augmented. Here, we focused on the hepatocellular form of DILI.
-
- Any drug exposure within 90 prior to the index date
-
- Laboratory values crossing threshold for DILI within 90 days after the drug exposure (the original phenotype also has a criteria of normal lab values prior to DILI. We didn’t include it since here the absence of test is likely equal to a normal test and only required the patients not to have abnormal tests before the index date).
-
- No condition of exclusion (Chronic liver injury, organ transplantation or liver operation, alcohol abuse/liver damage/toxic effects, viral hepatitis, death, overdose)
Informatics findings and discussion points:
-
- PHOEBE is useful in developing the set for acute liver injury, not only because of recommendations but mostly because it allows reviewing the concept set and spotting the commonly used yet not appropriate codes. For example, the ICD9CM code used in the original implementation 573.9 ‘Other specified disorders of liver’ is mapped to the broad ‘Disease of liver’, which we may want as a verbatim concept but don’t want all of its descendants.
-
- Creating the list of conditions of exclusion isn’t trivial either. Here, we basically include all of the chronic hepatocellular disorders even despite the fact that they can be present in DILI.
-
- Since we ran the algorithm on one data source, it was easy to get the list of measurements. Otherwise, it probably would’ve been more challenging both in terms of lab tests and their units.
We iterated over the cohort to remove other obvious reasons for liver injury and finally got 5,259 patients.
The top concepts were Zosyn, acetaminophen, atorvastatin, aspirin, lisinopril, prednisone, lorazepam, amlodipine.
At this point, we wanted to look at individual records, but it is impossible to review them all. Given the low prevalence, reviewing the records at random will likely miss the cases.
So, let’s find the cases (SNOMED 4055224 Toxic liver disease) and try to figure out
- a) If there are any features that can be used to refine the cohort
- b) If structured data is enough to establish causality compared to unstructured data
As you can imagine, patients have various age, co-morbidities and prior observation, have various time between liver injury and drug exposure.
A couple of examples:
Patient, F, 53yo: COVID-19, diabetes, acute respiratory failure with hypoxia, asthma, multiple drugs, transaminitis. In charts: Suspect DILI, possibly from clinical trial drug
Patient M, 59yo, chemotherapy, multiple myeloma, non-infectious diarrhea and transaminitis, a dozen of drugs that can cause DILI, resolved. In chart: DILI on melphalan
Patient, F, 68yo, glioblastoma, hypothyroidism, depression, osteoporosis, rash and transaminitis. On chemotherapy, antibiotics. In chart: potential DILI resolved.
Based on the examples, I would say that it’s really hard to establish DILI both in structured and unstructured data, especially for new drugs. It looks like we need better approaches for a) finding those potential associations and b) establishing a causal relationship between a drug and any rare adverse event.
I heard that some hospitals have procedures for reviewing and selecting charts with potential adverse events (done by humans), so that the final adjudication is done on a small sample. I wonder if and how we can scale and automate the process, so I would love to hear your thoughts (and read related papers).