Hello my fellow claims enthusiast, @Gowtham_Rao,  I’m not sure I know THE answer, but I can tell you what we have done to identify professional vs. facility claims for our internal use. We actually identify them at the condition/procedure level using type_concept_ids. When mapping ICD/CPT/HCPCS codes, from facility claims, we use the “inpatient header”, “inpatient detail”, “outpatient header”, and “outpatient detail” type_concept_ids (or ranges 38000184-38000244, 44818709-44818713 for condition_type_concept_ids). When mapping ICD/CPT/HCPCS codes from a physician claim, we use “carrier header” or “carrier detail” type_concept_ids (45756835-45756855 range for condition_type_concept_ids).
I’m not sure I know THE answer, but I can tell you what we have done to identify professional vs. facility claims for our internal use. We actually identify them at the condition/procedure level using type_concept_ids. When mapping ICD/CPT/HCPCS codes, from facility claims, we use the “inpatient header”, “inpatient detail”, “outpatient header”, and “outpatient detail” type_concept_ids (or ranges 38000184-38000244, 44818709-44818713 for condition_type_concept_ids). When mapping ICD/CPT/HCPCS codes from a physician claim, we use “carrier header” or “carrier detail” type_concept_ids (45756835-45756855 range for condition_type_concept_ids).
Since OHDSI’s standard for creating a visit record (i.e. from the patient’s perspective) could combine multiple types of claims (both professional and facility) into one visit_occurrence_id, we found it was best to identify facility vs. professional claim information at the condition/procedure level.
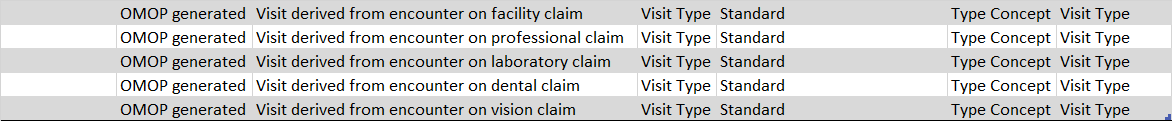
Your proposal for new visit_types are interesting and I love the idea. But it is a big departure from OHDSI’s original definition of a visit_occurrence (i.e. a visit a patient experienced - regardless of the number of procedures, claims, drugs that happened at that visit). This proposal is more in line with what we are doing internally, but we might want to see how the rest of the community feels about changing the definition of a visit (going from a patient experience to a claims-based account).
 or know of someone who have experienced this before.
or know of someone who have experienced this before.
 I’m not sure I know THE answer, but I can tell you what we have done to identify professional vs. facility claims for our internal use. We actually identify them at the condition/procedure level using type_concept_ids. When mapping ICD/CPT/HCPCS codes, from facility claims, we use the “inpatient header”, “inpatient detail”, “outpatient header”, and “outpatient detail” type_concept_ids (or ranges 38000184-38000244, 44818709-44818713 for condition_type_concept_ids). When mapping ICD/CPT/HCPCS codes from a physician claim, we use “carrier header” or “carrier detail” type_concept_ids (45756835-45756855 range for condition_type_concept_ids).
I’m not sure I know THE answer, but I can tell you what we have done to identify professional vs. facility claims for our internal use. We actually identify them at the condition/procedure level using type_concept_ids. When mapping ICD/CPT/HCPCS codes, from facility claims, we use the “inpatient header”, “inpatient detail”, “outpatient header”, and “outpatient detail” type_concept_ids (or ranges 38000184-38000244, 44818709-44818713 for condition_type_concept_ids). When mapping ICD/CPT/HCPCS codes from a physician claim, we use “carrier header” or “carrier detail” type_concept_ids (45756835-45756855 range for condition_type_concept_ids).