Good morning OHDSI!
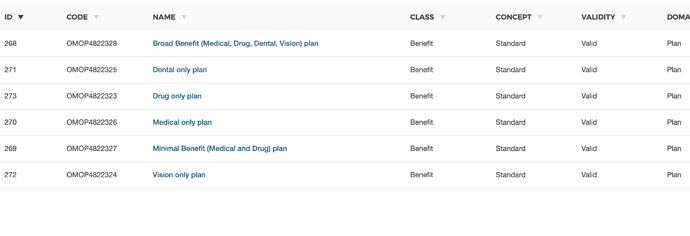
Payer plan period table needs your guidance for adding concept_id’s! This topic has been discussed before in the CDM work group, and in the forums.
GitHub https://github.com/OHDSI/CommonDataModel/issues/120 (approved by CDM WG).
Related discussions here and here thread.
We would like to begin adding vocabulary, but before adding wanted to get community opinion one more time
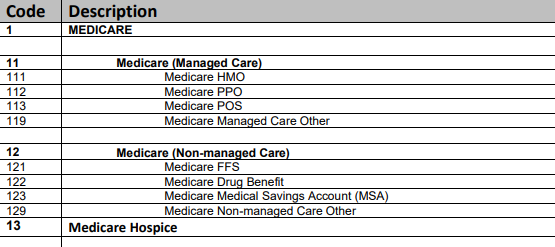
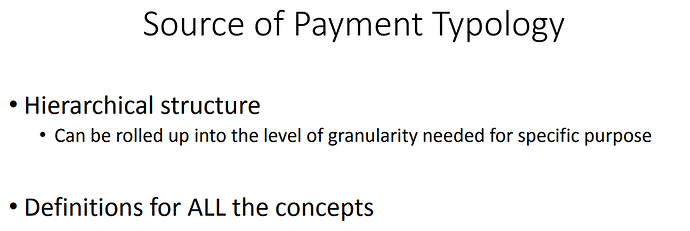
Question for discussion - Could we start by adding one vocabulary for the field payer_concept_id as the first vocabulary? i.e. can we add concept_ids for concepts in this external vocabulary pdf version and its corresponding csv versions are here for your review. Additional reading