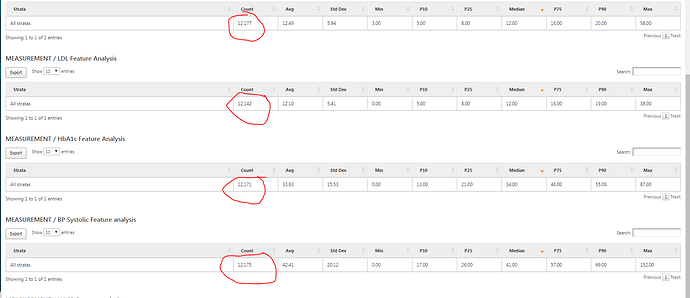
@Chris_Knoll Thank you for the response Chris. In addition, Can you let me know what happens when we generate the custom features for measurement values? I mean Systolic Blood Pressure, eGFR values. When I mean values, I talk about value_as_number field. So when I see the output as below and if they don’t indicate value_as_number field (came to know that from github) , can I know what does this result indicate or how to interpret this? 2 questions
-
When cohort size is 12177, why do I see different count for different features when we are generating features for the same cohort (which has 12177 records). Ex: LDL has only 12142 records. (Similar post here -
Atlas - Issue with Characterization display) -
What does Min (0.0) and Max (38.00) indicate in this scenario. We already have count.
I posted in github as well but thought of posting in forum as well for the use of community.