I have volunteered to organize the proposal for visits, encounters, care transitions, etc. under @Christian_Reich’s guidance. He suggested I gather all the interested parties and pertinent use cases, lead a discussion, put together a proposal based on our use cases, create a wiki, and then present it to the CDM WG.
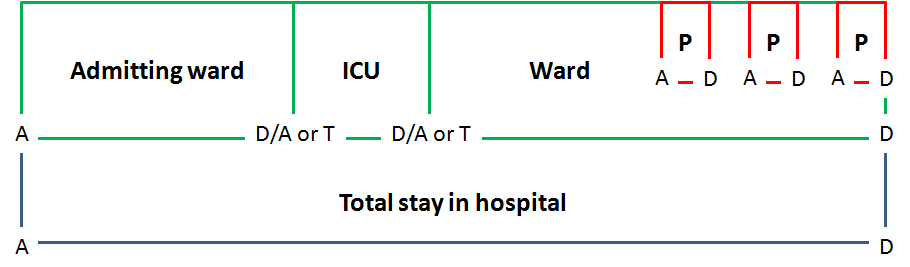
Our users request ADT data, specifically length of stay in a certain location (ward/unit) within the hospital, procedures that happen within a location within the hospital, and transfers between levels of care with the inpatient stay.
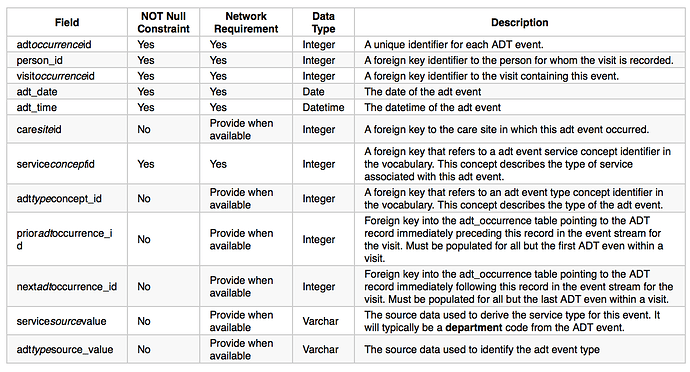
The only addition we would need for our use case to the PEDSnet table below would be the addition of an adt_occurrence_id FK to the PROCEDURE_OCCURRENCE table. This would allow us to link procedures to specific locations within the hospital.
These are the PEDSNet conventions for the above table. The conventions include an extension of the vocabulary to further define service_type and adt_type.
service_concept_id
select * from concept where vocabulary_id =‘PEDSnet’ and concept_class_id=‘Service Type’ and standard_concept=‘S’ yields 14 valid concept_ids.
In PEDSnet CDM v2.5, only the NICU,CICU and PICU services are included.
The value set available for PEDSnet includes:
• CICU (cardiac care) = 2000000079
• NICU (neonatal care) = 2000000080
• PICU (all other ICU) = 2000000078
• Critical care = 2000000067
• Intermediate care = 2000000068
• Acute care = 2000000069
• Observation care = 2000000070
• Surgical site (includes OR, ASC) = 2000000071
• Procedural service = 2000000072
• Behavioral health = 2000000073
• Rehabilitative service (includes PT, OT, ST) = 2000000074
• Specialty service = 2000000075
• Radiology = 2000000076
• Hospital Outpatient = 2000000077
li>Unknown: concept_id = 44814653
• Other: concept_id = 44814649
No information: concept_id = 44814650
adt_type_concept_id:
select * from concept where vocabulary_id =‘PEDSnet’ and concept_class_id=‘ADT Event Type’ yields 5 valid concept_ids.
The value set for PEDSnet includes:
• Admission = 2000000083
• Discharge = 2000000084
Transfer in = 2000000085
• Transfer out = 2000000086
Census = 2000000087
What are the other use cases? What is missing from the above? Who else is interested? Let’s get a proposal put together!
Melanie
Adding @bailey, @burrowse, @jenniferduryea, @Gowtham_Rao, @mgkahn