I created a package that runs any set of phenotypes defined on the public atlas server. (using utilities from Marc and Martijn). I made it a while ago for George’s cancer study but it can be re-used for other phenotypes as well.
So today I took Patrick’s atlas definition (the ID of it), added it to the a CSV file, ran package maintenance code. It can produce the estimates with no SQL coding or rendering needed.
I suggest any site uses this package to get cohort counts. (and please report results how the package worked back in this forum).
Here is the package full URL and readme instructions:
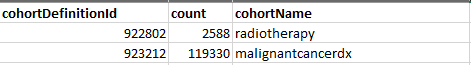
The output file looks like this: (with two previous phenotypes shown only)
The settings file now has egfr phenotype. See it here: StudyProtocolSandbox/CancerTreatments/inst/settings/CohortsToCreate.csv at master · OHDSI/StudyProtocolSandbox · GitHub
So our network already has a nice mechanism how to quickly generate multiple phenotypes cohort extimate. Use that package. I am planing improvements to compute “table 1” for each phenotype using Feature Extraction package.