thanks @Christian_Reich very useful and yes @Pulver if we have height, weight, or BMI we can get a little more accurate with estimating the eGFR.
If we do not have height, weight, etc. then perhaps we can use race/ethnicity proxies - but again there are issues with that…but i agree with several of you that have noted that using one skin surface measure for all datasets in the world is not a good approach
Good idea by @Pulver, but the point here is not to use the actual skin surface. In other words, it is not important if a person is fat or skinny. The thing is that the physiological eGFR is proportional to the square of height, so they use the 1.73 m2 as an artificial benchmark. Most eGFR calculators don’t even ask for height, only for children.
Hi Mary, hope all is well! I also want to add that from clinical epi
perspective, the eGFR estimation via MDRD, CKD-EPI, and Cockgroft-Gault
don’t always match. Not sure if the estimation methods are all represented
in the data model (I see MRDR above).
I think this goes back to whether you want to estimate directly from Cr
which is a direct measurement.
Best,
Kye
A lot of eGFR calculators don’t ask for height, but then they make adjustments based on race/ethnicity, etc. - so there might be some height adjustment baked into those formulas (even if they don’t adjust directly for height)
Better to have creatinine clearance, height and race/ethnicity - then the estimated GFR would be closer to the ‘true’ GFR…however, its important to note that all of the eGFRs are estimated…better to use the ‘raw’ creatinine clearance values - unless the actual challenge data is obtainable (which would be ideal)…
Well, it is for children: http://www.calculator.net/gfr-calculator.html.
For adults the variation in height is not that great, so most places don’t bother. It’s not that an exact measurement anyway. It gives you corridors of renal impairment:
Kidney damage stage description estimated gfr (ML/MIN/1.73M2)
1 Normal or minimal kidney damage with normal GFR 90+
2 Mild decrease in GFR 60-89
3 Moderate decrease in GFR 30-59
4 Severe decrease in GFR 15-29
5 Kidney failure <15
@Christian_Reichhttp://forums.ohdsi.org/users/christian_reich
So by coalescing actual height with a default of 1.73m, we’d get slightly more accurate estimate for those subjects for whom we have height and be no worse off for the others.
Thanks,
Gerry
agreed - use actual height when possible otherwise use some default height…
I created a package that runs any set of phenotypes defined on the public atlas server. (using utilities from Marc and Martijn). I made it a while ago for George’s cancer study but it can be re-used for other phenotypes as well.
So today I took Patrick’s atlas definition (the ID of it), added it to the a CSV file, ran package maintenance code. It can produce the estimates with no SQL coding or rendering needed.
I suggest any site uses this package to get cohort counts. (and please report results how the package worked back in this forum).
Here is the package full URL and readme instructions:
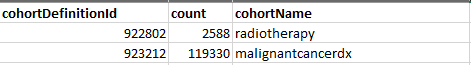
The output file looks like this: (with two previous phenotypes shown only)
The settings file now has egfr phenotype. See it here: StudyProtocolSandbox/CohortsToCreate.csv at master · OHDSI/StudyProtocolSandbox · GitHub
So our network already has a nice mechanism how to quickly generate multiple phenotypes cohort extimate. Use that package. I am planing improvements to compute “table 1” for each phenotype using Feature Extraction package.
A couple of quick comments from a clinical perspective here (disclaimer: internist, not a nephrologist)
-
RE: measurement of true GFR. Rarely done. I’ve only seen it done in pre- kidney transplant evaluations. Uptodate mentions it might be done in some areas of chemotherapy due to narrow therapeutic windows of a particular drug, I’ve not seen it used in that context.
-
RE: eGFR. I believe an assumption in all equations is that the creatinine is in steady state. If you’re going to use eGFR measures in a study, you’d want to parameterize any particular measure to ensure you aren’t evaluating this in the context of a kidney injury and dynamically changing renal function.
Checking on a Cr measurement before and after (a suitable delta time) to ensure you’re in a ‘steady state’ would be way to implement in practice?
This assumes the research use case does really need eGFR.
I do see a reasonable count in Stanford Stride v6 but none in v7 - I can ask around as to why this is if there’s something moving forward…
Evan
thanks @Evan_Minty: all good points.
I agree that true GFR is probably rarely done - however, the algorithm will probably extract it if it is present (again this might only be useful for data coming from cancer centers). I do believe the context of the measurements is important. Also regarding steady state, that may be tricky in EHRs where there is often a degree of missing-ness. However, I think it will be possible to design an algorithm that addresses this issue. We are working on finalizing the study - and hope to launch in the near future…so if you could find out about increased data accessibility in the interim that would be great.
Thanks!
