@Gowtham_Rao, @bnhamlin, @Daniella_Meeker and whoever else may be interested in applying OHDSI to use cases around quality improvement:
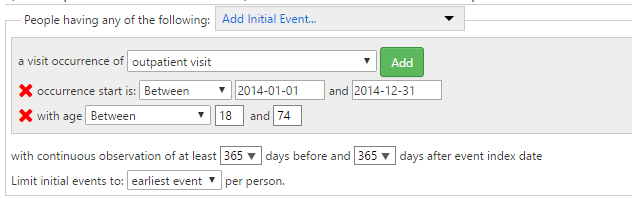
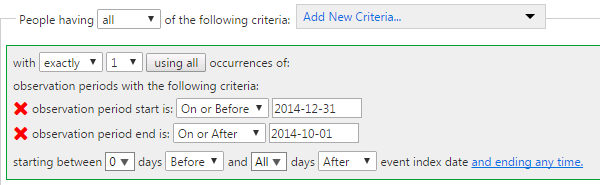
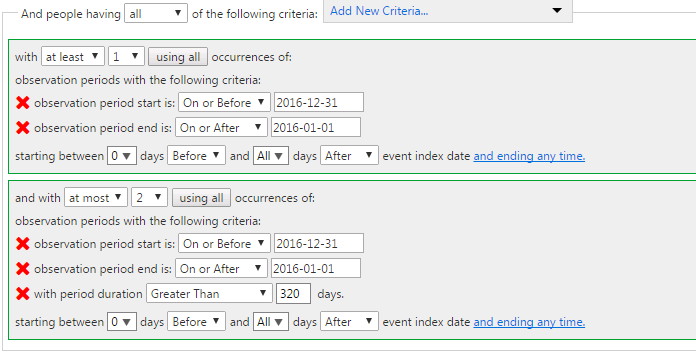
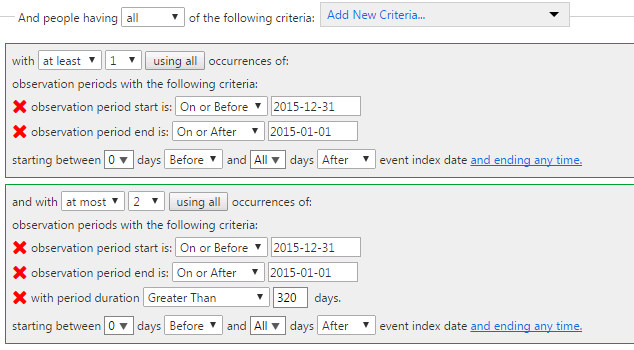
As a quick demonstration, I created two instances of the HEDIS measure of ‘BMI Assessment’ (ABA) in ATLAS:
-
Using standard concepts (which provides a much more efficient manner of defining the value sets, and seems to sweep in extra ICD9/10 codes that should have been captured but are apparently missed): http://www.ohdsi.org/web/atlas/#/cohortdefinition/87847
-
Using source concepts that define the valuesets for BMI and BMI percentile, just to demonstrate how ATLAS can create cohorts using source concepts instead of standards (even though, as a general principle we discourage this behavior): http://www.ohdsi.org/web/atlas/#/cohortdefinition/87846
I’ll post to this thread as I go through and do more. As I read the measures, I haven’t yet encountered anything I think can’t be directly supported within ATLAS given all of the enhancements that @Chris_Knoll has made to the standard cohort definition module. There’s a minor bug around observation_period that appears to have been introduced in the last release, but I expect Chris will have a hoxfix for that shortly. I’ll be curious if others tried to use ATLAS and have found specific limitations, in which case, please post to this thread so we can learn.