Let me make a few remarks.
I find the term open and closed confusing. Pre-adjudication and adjudicated (or adjudication-completed or post-adjudication) is better.
Even better - you say source and adjudication status
So types are:
- FromProvider~pre-adjudication
- FromPayer~pre-adjudication
- FromPayer~completed-adjudication
Payer pays only for procedures. Not diagnoses. So to simplify, I will focus on duo of tables ‘cost’ and ‘procedure_occurrence’.
The types below seem like not be enough.
OMOP4822212 Provider System Open Claims
OMOP4822218 Payer system (Primary payer) Closed Claims
OMOP4822217 Payer system (Secondary payer) Closed Claims
First addition must by origin of the claim (professional vs facility vs dental) (and it was pointed out in this thread)
Second addition is the RESULT OF ADJUDICATION. (accepted-and-paid vs. rejected) for Closed (=adjudication-complete) Claims.
Consider a case A) where provider performed to patient a cervicoplasty (plastic surgery procedure on the neck) (CPT 15819).
From patient point of view the procedure happened. But if result of adjudication is rejection – depending on ETL rules, it may end up in CDM or it may not. I would like to see how various groups represent rejection/acceptance of a claim by payer.
You need to split code OMOP4822218 Payer system (Primary payer) Closed Claims into two flavors
- OMOP48222181 Payer system (Primary payer) Closed Claims – Rejected by Adjudication
And
- OMOP48222182 Payer system (Primary payer) Closed Claims – Accepted by Adjudication
If you have secondary Payer – it may be referred to that secondary payor and result of secondary payer adjudication may be Accepted. So do you put the row there twice?
No -because we are patient centric but with some eye on at least good-enough (or allowed in OMOP) claim-ish-ness – you can create a third code for claim type that says ‘rejected by primary and accepted by secondary’ (as postcoordination).
Going back to conditions linked to type of source data of FromPayer~pre-adjudication – what do you do with diagnoses for a claim where all procedures on that claim were rejected?
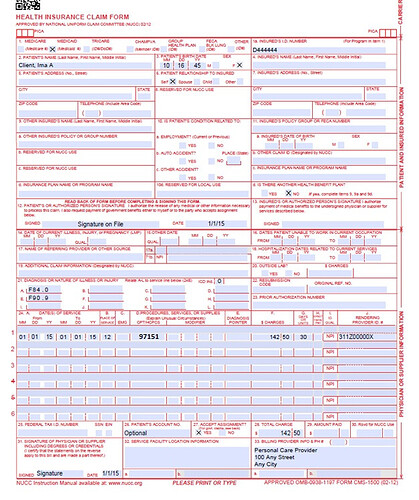
For reference, claim form example pasted below (from here)
Result of adjudication is absolutely key for ‘cost’ table so our type concepts at the moment are ‘not fit for purpose’ for patient centric model that also tries to be as claim-ish as possible at the same time. And in my view, why not allow it. Type concept hierarchies is what we used in other situations.