Hi all!
If I want to add record with patient payment what cost_type_concept_id value should I choose?
I see 3 standard concept_ids:
31968 - Payer is primary (coordination of benefit)
31969 - Payer is secondary (coordination of benefit)
31970 - Premium
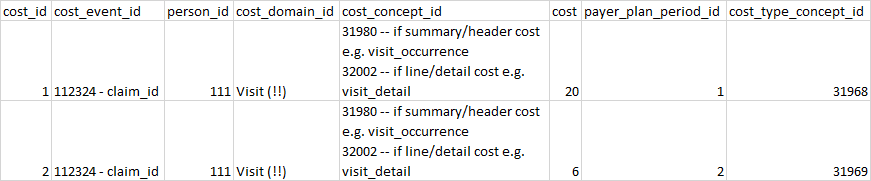
So I have to choose 31969 for patient payment if part of the bill amount has to be paid by insurance company and I have to choose 31968 if only patient has to pay the bill. Is it correct?
For example:
Case 1:
Total bill: $100
Insurance company1: $70
Insurance company2: $20
Patient: $10
For patient payment choose 31969 - Payer is secondary (coordination of benefit)
Case 2:
Total bill: $15
Patient: $15
For patient payment choose 31968 - Payer is primary (coordination of benefit)
Thank you in advance

 So we may want to add in some cost_type_concept_ids that are CDM 5.3 compliant.
So we may want to add in some cost_type_concept_ids that are CDM 5.3 compliant.